Atherosclerosis and Cardiovascular Disease
Atherosclerosis and Cardiovascular Disease
Last Section Update: 10/2022
Contributor(s): Maureen Williams, ND; Colleen Mazin, MS/MPH; Debra Gordon, MS; Carrie Decker, ND, MS; Shayna Sandhaus, PhD
1 Overview
Summary and Quick Facts for Atherosclerosis and Cardiovascular Disease
- Atherosclerosis can occur anywhere in the body, but it is particularly dangerous when it affects the arteries that supply oxygenated blood to the heart muscle. This is called coronary artery disease (CAD), and is the most common type of heart disease, affecting 16.5 million Americans.
- Scientific studies have revealed that several nutrients effectively protect against endothelial dysfunction caused by atherogenic factors. Unlike mainstream medicine’s approach to treating atherosclerosis, which involves addressing only very few proven cardiac risk factors, a comprehensive nutritional regimen can be designed to target all of the risk factors that contribute to atherosclerosis.
- Comprehensive blood testing helps aging individuals identify and target their specific risk factors, allowing for the development of a personalized, targeted treatment regimen that can be used to preserve and improve cardiovascular health.
What is Atherosclerosis?
Atherosclerosis is the narrowing and hardening of arteries due to the accumulation of plaque. If left unchecked, atherosclerosis can lead to cardiovascular disease, the deadliest disease in the United States. Unfortunately, many people simply focus on reducing a few of the risk factors, such as cholesterol and high blood pressure, yet ignore a host of other risk factors.
The underlying cause for all cardiovascular disease is endothelial dysfunction. Endothelial cells line the inside of arteries, and over time they are exposed to atherogenic factors and become damaged. When the endothelial cells cannot function properly, plaque builds up and calcifies, narrowing the artery.
Natural interventions such as quercetin and omega-3 fatty acids can help protect endothelial function and fight cardiovascular disease.
What are Risk Factors for Atherosclerosis and Cardiovascular Disease?
- Elevated LDL cholesterol and low HDL cholesterol
- Elevated triglycerides
- Hypertension
- Elevated glucose and insulin levels
- Insufficient vitamins D and K
- Hormonal imbalances
- Smoking
- Obesity, and others
What are the Signs and Symptoms of Atherosclerosis?
Atherosclerosis is generally asymptomatic until very late stages. It is therefore critical for all aging individuals to take preventative measures and visit a doctor regularly.
What are the Conventional Medical Treatments for Atherosclerosis?
- Cholesterol-lowering drugs
- Blood pressure-lowering drugs
- Angioplasty and stents
- Surgery (coronary artery bypass), and others
What Dietary and Lifestyle Changes Can Benefit Atherosclerosis?
- Consider low-dose aspirin therapy
- Eating a balanced diet rich in fruits and vegetable (Mediterranean style diets can be beneficial)
- Exercise regularly
- Quit smoking
- Limit alcohol intake
What Natural Interventions Can Benefit Atherosclerosis?
- Omega-3 fatty acids. Omega-3 fatty acids help to prevent the development and progression of cardiovascular disease through multiple mechanisms including lowering triglycerides, lowering blood pressure, improving endothelial function, and raising HDL levels.
- L-arginine. This amino acid is a precursor of nitric oxide, a vasodilator. Treatment with L-arginine improved brachial artery dilation, a measure of endothelial function, in patients with coronary artery disease.
- Coenzyme Q10 (CoQ10). CoQ10 is involved in the production of ATP, the energy currency in the human body. Treatment with CoQ10 improved vascular endothelial function in patients with atherosclerosis or significant risk factors for atherosclerosis.
- Lipoic acid. Lipoic acid is an antioxidant that serves as a coenzyme in energy metabolism of fats, carbohydrates, and proteins. It improved endothelial function in patients with metabolic syndrome.
- Quercetin. Quercetin is a polyphenol with antioxidant and anti-inflammatory properties. Quercetin supplementation has been linked to improved measurements of inflammation in patients with high blood pressure.
- Niacin. Niacin can improve cholesterol profile and endothelial function. Heart attack survivors who took niacin supplements had reduced recurrence of heart attacks and incidence of stroke.
- Lactobacillus reuteri 30242. This probiotic strain, and other Lactobacillus strains, have been shown to support cardiovascular health.
- Other natural interventions that can aid in preventing atherosclerosis and cardiovascular disease include propionyl L-carnitine, garlic, ginkgo biloba, resveratrol, vitamins C, K, and E, hesperidin, and others.
2 Introduction
Atherosclerosis is a long-term disease process in which arteries narrow and stiffen due to the accumulation of plaque.1,2 This plaque, made up of cholesterol, cellular waste products, blood clotting materials, and fatty substances, builds up in the lining of the arteries and restricts blood flow.1 As atherosclerosis progresses, these plaques may rupture or break apart, which can cause a blood clot. This can lead to serious complications such as a heart attack or stroke.2
Atherosclerosis can occur anywhere in the body, but it is particularly dangerous when it affects the arteries that supply oxygenated blood to the heart muscle. This is called coronary artery disease (CAD), and is the most common type of heart disease, affecting 16.5 million Americans.3 About 20% of American men and 13% of women aged 60 to 79 years have CAD, and the prevalence increases with age: 31% of men and 25% of women over age 79 have CAD.4,5 However, atherosclerosis is not confined to older people; the atherosclerotic process can begin as early as adolescence.2,6
Many factors contribute to the development of atherosclerosis, some of which are modifiable. Lifestyle factors that can increase the risk of atherosclerosis include being overweight, poor diet and lack of physical activity, smoking, and excessive alcohol consumption. Factors that can damage the delicate lining of the arteries (called the endothelium) and contribute to atherosclerosis include elevated blood pressure, high cholesterol and/or triglycerides, diabetes and insulin resistance, and inflammation.1 Non-traditional risk factors that strongly correlate with atherosclerosis include blood levels of homocysteine and C-reactive protein (hs-CRP).7-10 Tracking both traditional and non-traditional risk factors through periodic blood testing can help you monitor your overall vascular health and plan your diet, lifestyle, and nutrient supplementation regimen accordingly.
In this protocol, you will learn how atherosclerosis develops and contributes to potentially deadly cardiovascular events. You will also learn how you can use blood testing and other strategies to assess your cardiovascular risk. This protocol will also help you understand the different medical options available to treat vascular disease, and how dietary and lifestyle changes, along with targeted nutritional supplementation, can help support overall cardiovascular health.
Because cardiovascular health is influenced by a variety of factors, readers should also review Life Extension’s protocols on Cholesterol Management, High Blood Pressure, Homocysteine Reduction, Stroke , Blood Clot Prevention, Weight Loss, and Diabetes and Glucose Control.
3 How Atherosclerosis Develops
Atherosclerosis develops over many years. During the course of the disease, several changes occur in the arteries, culminating in arterial plaques that may rupture and cause major cardiovascular events such as heart attack or stroke.11
Endothelial cells are critical to the health and function of blood vessels. They line the inside of vessels and help facilitate healthy blood flow. In atherosclerosis, injury causes the endothelial cells to become dysfunctional and produce proteins that attract circulating immune cells called monocytes. The monocytes enter the blood vessel lining and transform into macrophages. Macrophages are specialized cells whose role is to engulf and destroy infectious agents, cancer cells, or other unhealthy substances. The macrophages become so-called “foam cells” by absorbing excess fatty deposits on the blood vessel walls, including low-density lipoproteins (commonly known as LDL). As macrophages become filled with lipids, they develop a foamy appearance.12,13
Foam cells can also derive from vascular smooth muscle cells, which exist in normal blood vessels just below the endothelium (the lining of the blood vessels) and are responsible for contraction and relaxation of blood vessels. They can change their cell type to become more like macrophages and, ultimately, foam cells.14
The accumulation of foam cells, along with the proliferation of smooth muscle cells and excess connective tissue, are key drivers of atherosclerosis. Fortunately, the accumulation of foam cells is a reversible process, and a reduction of foam cells is associated with an improvement in the size of atherosclerotic plaque.15
Phases of Atherosclerotic Plaque Development
The formation of atherosclerotic plaque begins with injury to the blood vessel lining, or endothelium. Many conditions can lead to endothelial injury.16 For example, elevated levels of certain blood lipids, such as oxidized low density lipoproteins (ox-LDL), can damage endothelial cells, as can high blood pressure and pro-inflammatory biochemicals.
Intimal thickening. During intimal thickening, the inner layers of blood vessels (ie, the intima) thicken. Intimal thickening, which is the earliest vascular change in atherosclerosis, can be seen with a microscope. It mainly consists of the accumulation of smooth muscle cells and extracellular matrix (non-cell components of body tissue).17
Fatty streak formation. Fatty streaks are so named because they can be seen by the naked eye at autopsy as irregular, yellowish streaks on the inside of blood vessels. Fatty streaks are considered an early sign of atherosclerosis and may be observed as early as childhood. They have even been detected in human fetal aortas and are increased in number and size if the mother has high cholesterol.18 Fatty streaks can progress to full-developed atherosclerosis or may sometimes regress with healthy dietary and lifestyle changes.19
Fibro-calcific plaque formation. Atherosclerosis that progresses beyond the fatty streak phase is characterized by fibrous plaques, which are growths that can restrict blood flow. They are composed of a thick (fibrous) cap that encapsulates cellular debris.20 The collection of cellular debris within the fibrous plaque is referred to as the necrotic core.
Atherosclerotic plaques can also become depots for abnormal calcium accumulation.20 In advanced atherosclerosis, plaques begin to calcify via both active and passive processes. In fact, some of the processes by which calcium accumulates in arterial plaques resemble those involved in bone formation. Degree of vascular calcification correlates with the risk of major adverse cardiovascular events.21-25
Vulnerable plaque. Atherosclerotic plaques are considered vulnerable when they are prone to rupture. Plaque rupture is the most common cause of heart attacks, near heart attacks (unstable angina), and sudden death. These outcomes occur when a coronary artery is suddenly blocked and therefore cannot supply enough blood to the heart muscle. The underlying mechanism is the formation of a blood clot within the blood vessel, known as thrombosis. Thrombosis mostly occurs in association with plaque rupture; less often, blood clots form around plaque erosions or calcified nodules.17 Plaques that rupture can cause blood clots that block blood flow or break off and travel to another part of the body, known as an embolism. If a blood clot blocks a vessel to the heart, it causes a heart attack. If a blood clot blocks a vessel that goes to the brain, it causes a stroke.26
Certain conditions are associated with softening of the cap’s strength, making it more likely that the cap will burst. These conditions include increased shear stress (due to high blood pressure), calcium and iron deposition, and an increase in macrophage-derived enzymes called matrix metalloproteinases, which lead to the breakdown of the extracellular matrix.17 Hemorrhage (bleeding) within the core may also make a fibrous plaque more vulnerable. Over time, a fibrous plaque’s core may be subject to small hemorrhages. These hemorrhages are more commonly observed at autopsy in ruptured plaques than intact plaques.17
Please see Life Extension’s protocol on Blood Clot Prevention for more information.
4 Atherosclerosis: Signs, Symptoms, and Diagnosis
Atherosclerosis rarely causes signs or symptoms until there is severe artery blockage. Many people are unaware that they have the disease until they suffer from a cardiac event such as stroke or heart attack. When plaque develops in a coronary artery (the arteries that supply oxygenated blood to the heart), angina (chest pain), shortness of breath, and irregular heartbeat may occur. Plaque in smaller coronary arteries may also cause sleep problems and fatigue.27
When plaque develops in the carotid arteries, which are the arteries that supply oxygenated blood to the brain, stroke symptoms may develop, including weakness, confusion, problems breathing or moving, dizziness, and headaches. Atherosclerosis in the peripheral arteries (which supply blood to the legs, arms, and pelvis) may cause numbness and pain, and in the renal (kidney) arteries, it may cause chronic kidney disease and decreased kidney function.27
Diagnosis occurs after a physical exam, where the doctor may check your pulse and listen to your arterial function. Other diagnostic tests include:
- blood tests for lipids and inflammatory markers;
- a chest X-ray to visualize heart failure;
- an electrocardiogram to detect the heart’s electrical activity;
- an echocardiogram to determine the size and shape of the heart and identify poor blood flow or irregular muscle contractions in the heart;
- computed topography (CT) scanning to display hardened or narrow arteries in the heart;
- stress test to show abnormal changes in heart rate or blood pressure during exercise, and provide imaging of blood flow in the heart;
- angiography, magnetic resonance imaging (MRI), and positron emission tomography (PET) to help visualize arterial plaque.27
5 Atherosclerosis Risk Factors
The development of atherosclerosis is a complex process, and it has many risk factors. This section highlights several of the key risk factors known to contribute to the development of atherosclerosis and increase risk of cardiovascular disease. In addition, this section discusses numerous biomarkers that correlate to varying degrees with atherosclerotic burden and/or risk of cardiovascular events.28 Many of these risk biomarkers can be measured and tracked through periodic blood testing to help monitor disease risk. Some of these biomarkers can be normalized or at least improved in most cases with dietary and lifestyle changes, medications, and/or nutritional supplements.
For a greater understanding of the factors that influence cardiovascular health, refer to Life Extension’s protocols on Cholesterol Management, High Blood Pressure, Homocysteine Reduction, Stroke, Thrombosis Prevention, and Diabetes and Glucose Control. For more information about cardiovascular risk biomarkers, please see the Life Extension Magazine article titled How to Circumvent 17 Independent Heart Attack Risk Factors.
Obesity
Obesity is a chronic disease characterized by the accumulation of visceral and subcutaneous fat. It is associated with an increased risk of several diseases, including cardiovascular and metabolic conditions. Excess body fat (especially abdominal fat ) is linked to atherosclerosis by a number of mechanisms.29 For instance, fat cells produce leptin, high levels of which can contribute to endothelial dysfunction, increased inflammation, high blood pressure, and thrombosis.30 Fat cells also produce reactive oxygen species (ROS) and contribute to oxidative stress, which is in turn linked to obesity and insulin resistance.31
When abdominal obesity is present alongside high blood sugar, low HDL, high triglycerides, and high blood pressure, it creates a condition called metabolic syndrome.32 Whether metabolic syndrome imparts more risk of atherosclerosis than the sum of its parts is unclear, but metabolic syndrome is associated with increased mortality risk, both from cardiovascular disease and all causes.33,34
Poor Diet
Research has long linked diet with the progression of atherosclerosis.35 Excess calories, fat, sugar, and cholesterol all play a role in cardiovascular disease promotion. A diet high in saturated fat and cholesterol may raise cholesterol levels, which may increase the amount of plaque in the arteries. Epidemiological research suggests that consuming fruits and vegetables may reduce the risk of atherosclerosis and coronary artery disease.36
The American Heart Association recommends a diet that includes a variety of fruits and vegetables, whole grains, low-fat dairy, lean poultry and fish, nuts and legumes, and non-tropical vegetable oils, such as canola, olive, and corn oil. In addition, saturated fats, trans fats, sodium, sugar, and red meats should be limited.37
Please see the “Adopt a Healthy Diet” section later in this protocol for more information.
Lack of Physical Activity
The link between physical activity and cardiovascular health was first established in the early 1950s, and research has since consistently found that high levels of physical activity are associated with reduced risk of CHD morbidity and mortality.38 Research suggests that in both men and women, there is an inverse relationship between physical activity and cardiovascular disease, and this relationship persists after control for other risk factors.39 One older study involving nearly 17,000 men found that those who maintained a moderately vigorous exercise habit had a 28% reduction in mortality from all causes over a 16-year follow-up period compared with sedentary men.39 Maintaining or increasing physical activity level in late middle age was associated with a reduction in mortality rates, and light activities appeared to be sufficient to produce this benefit in older men.40 Among people with established cardiovascular disease, mortality is lower among those who participate in an exercise program than among those who do not.41
Regular exercise combats atherosclerosis by reducing the amount of fat circulating in the blood, lowering blood pressure and cholesterol levels, and helping maintain a healthy weight.42 See the “Be Active” section for more information.
Cigarette Smoking
Tobacco use is a major modifiable risk factor for many diseases, including cardiovascular diseases such as coronary artery disease, stroke, vascular disease, and congestive heart failure. Smoking cigarettes is known to damage the heart and blood vessels as well as elevate cholesterol and blood pressure levels. It also prevents oxygen from adequately reaching all of the body’s organs and tissues.27 Smokers have elevated levels of ROS, cell adhesion molecules, and pro-inflammatory biochemicals. Smokers also have excess intimal thickening of the carotid artery, even when the results are statistically controlled to eliminate other atherosclerosis risk factors.43
For more information, see the section titled “Avoid Tobacco Use and Second-hand Exposure.”
Age and Family History
Aging is the dominant risk factor for clinically significant atherosclerotic lesion formation.44 Risk increases after age 45 in men and 55 in women. Plaque buildup that has been occurring for many years as a result of genetic factors, poor diet, and lack of physical activity may begin to cause health problems during middle-age.27
Family history is also an important risk factor for atherosclerosis, as an individual’s risk increases if their father or brother was diagnosed with heart disease before age 55 or if their mother or sister was diagnosed before age 65.27 A prospective trial with over 5,000 subjects found that a family history of premature coronary heart disease is associated with the progression of coronary artery calcification. The greatest risk was with a combined parent and sibling history.45
Elevated Blood Lipids (Cholesterol and Triglycerides)
Cholesterol is a wax-like steroid molecule that plays a critical role in metabolism. It is a major component of cellular membranes and serves as a precursor to a variety of steroid hormones in the body. Cholesterol is also the precursor to vitamin D and provides the framework for the synthesis of bile acids, which emulsify dietary fats for absorption.46
Low-density lipoproteins (LDLs) carry cholesterol from the liver to cells that require it. In aging people, LDL often transports cholesterol to the linings of their arteries, where it may not be needed. Because of the correlation between elevated blood levels of cholesterol carried in LDL and the risk of heart disease, LDL is commonly referred to as “ bad cholesterol.” Ox-LDL is a particularly damaging form of LDL that can infiltrate and damage arterial walls and lead to the development of lesions and arterial plaques.13,47 Another process, called glycation, can also modify LDL particles and make them more atherogenic. LDL glycation occurs when a sugar molecule modifies the LDL structure. LDL glycation can play a direct role in the development of atherosclerosis and may also make the LDL more prone to oxidation.48
High-density lipoproteins (HDLs) transport excess cholesterol back to the liver, where it can be re-processed and/or excreted from the body. HDL can remove excess cholesterol from the arterial wall.46,49
Triglycerides also play a role in atherosclerosis. High triglycerides can decrease HDL levels and increase oxidative stress and the production of pro-inflammatory biochemicals. High triglycerides can also lead to the production of small, dense LDL, a subtype of LDL that is more atherogenic than larger, more buoyant LDL. In addition, high triglycerides can increase blood clot risk by increasing production of certain clotting factors.13 Research indicates that elevated non-fasting triglyceride levels (blood draws completed two to eight hours after a meal), even more so than fasting triglyceride levels (blood draws done 12 hours after eating), may be associated with increased risk of heart attack and stroke.50
Maintaining healthy cholesterol and triglyceride levels is a key factor in cardiovascular risk reduction. Lowering serum cholesterol to a healthful range—total cholesterol about 160–180 mg/dL and LDL cholesterol ideally 40 — 80 mg/dL—is an important strategy for managing heart disease risk.46 For young adults (age 20‒39), a 2018 expert panel recommended cholesterol-lowering therapy for those with LDL cholesterol over 160 mg/dL and a history of early-onset atherosclerosis in a close family member. For older adults, cholesterol-lowering therapy should be considered if one has diabetes, an LDL concentration ≥ 190 mg/dL, or increased risk as determined by a risk algorithm.51
Life Extension recommends a fasting blood triglyceride level under 80 mg/dL for anyone with any cardiovascular risk factors and under 60 mg/dL for people with a history of cardiovascular disease. The optimal target for non-fasting triglycerides is under 116 mg/dL. While triglyceride levels can be lowered with prescription medications, nutrient options include fish oil, niacin, green tea, and soy protein supplementation.52-56 Weight loss, caloric reduction, a diet rich in fruits and vegetables, and physical activity also promote cardiovascular health.
Please see Life Extension’s protocol on Cholesterol Management for more information.
High Blood Pressure
Blood pressure is the measurement of systolic pressure (maximum pressure during one heartbeat) over diastolic pressure (minimum pressure between heartbeats). Healthy blood pressure is less than 120/80 mm Hg, and Life Extension recommends an optimal target of 115/75 mm Hg. High blood pressure is an established risk factor for overall cardiovascular disease, and atherosclerosis in particular. Observational evidence suggests the risk of cardiovascular disease doubles for each increment of 20 mm Hg systolic and 10 mm Hg diastolic above 115/75 mm Hg.57
A large, randomized, controlled trial with over 9,300 subjects showed that non-diabetics at increased cardiovascular risk can substantially reduce their risk of cardiovascular events and death by lowering their blood pressure.58,59 One group of trial participants was intensively treated with blood-pressure-lowering medications to a target systolic blood pressure of less than 120 mm Hg. The other group received medications with a treatment goal of achieving systolic blood pressure of less than 140 mm Hg. The intensively treated subjects took, on average, one additional blood pressure medication compared with the standard treatment group. The trial was scheduled to last for five years, but was stopped after a median of only 3.3 years of follow-up because subjects who underwent more intensive blood pressure lowering had a dramatic 25% risk reduction for a composite of cardiovascular outcomes and a 27% lower risk of death from any cause compared with the standard-treatment group.59
Note: Blood pressure treatment goals may need to be adjusted based on baseline risk and health status (eg, diabetes status). See “Managing Blood Pressure” later in this protocol for a discussion of treatment goals in people with established cardiovascular disease or otherwise at high risk.
Antihypertensive medications may be prescribed to lower blood pressure levels, but nutrients such as garlic, coenzyme Q10 (CoQ10), fish oil, and vitamin C may also be used.60-63 In addition, modifying lifestyle factors such as adopting the Dietary Approaches to Stop Hypertension (DASH) diet, which includes a variety of fruits and vegetables and restricted salt intake, exercising, and quitting smoking also support healthy blood pressure levels.
More information, including summaries of several additional nutritional interventions to support healthy blood pressure, is available in Life Extension’s High Blood Pressure protocol.
High Blood Sugar, Insulin Resistance, and Diabetes
Research suggests fasting glucose levels over 85 mg/dL incrementally increase heart attack risk.64 Diabetes is a strong risk factor for atherosclerosis, and is associated with an accelerated form of the disease. Hyperglycemia (elevated blood sugar) activates inflammatory pathways in the body, increases the production of cell adhesion molecules, and reduces the production of nitric oxide, a naturally occurring biochemical that lowers blood pressure and increases blood flow.65
Insulin, a hormone that regulates blood sugar levels, allows the body to use or store glucose from food. Excess insulin in the blood (due to aging, genetics, poor diet, and/or physical inactivity) reduces the ability of cells to absorb and utilize glucose. When muscle, fat, and liver cells do not respond to insulin, the pancreas makes more, which further contributes to insulin resistance.66 Excess insulin is associated with an increased risk of heart attack, stroke, and cancer.67 Life Extension recommends target blood levels of fasting insulin under 5 µIU/mL.
Glucose control and insulin signaling can be improved through the use of pharmaceuticals such as metformin, increasing soluble fiber in the diet, supplements such as chromium, cinnamon, and L-carnitine, and adhering to healthy eating plans such as the Mediterranean diet.68-72
Please see Life Extension’s protocol on Diabetes and Glucose Control for more information
Periodontitis (Gum Disease)
Inflammatory gum disease is an established risk factor for atherosclerosis.73 Periodontitis allows bacteria into the bloodstream, resulting in an inflammatory response that contributes to atherosclerosis. Treatment of periodontitis has been shown to improve markers associated with cardiovascular health, such as hs-CRP blood levels and endothelial function.74
More information is available in Life Extension’s Oral Health protocol.
Other Health Conditions
Diseases that involve chronic inflammation can also increase risk of atherosclerosis and cardiovascular disease.75 Autoimmune inflammatory diseases like rheumatoid arthritis and systemic lupus erythematosus are associated with an increased risk of death from cardiovascular disease. The link between autoimmune diseases and cardiovascular disease is partly intuitive: inflammatory biochemicals that can promote inflammation in the blood vessel are elevated in autoimmune diseases. Additionally, HDL cholesterol is less protective in those with certain autoimmune diseases. HDL dysfunction has also been shown to occur in viral and bacterial infections in animal models.75
Unhealthy Microbiota
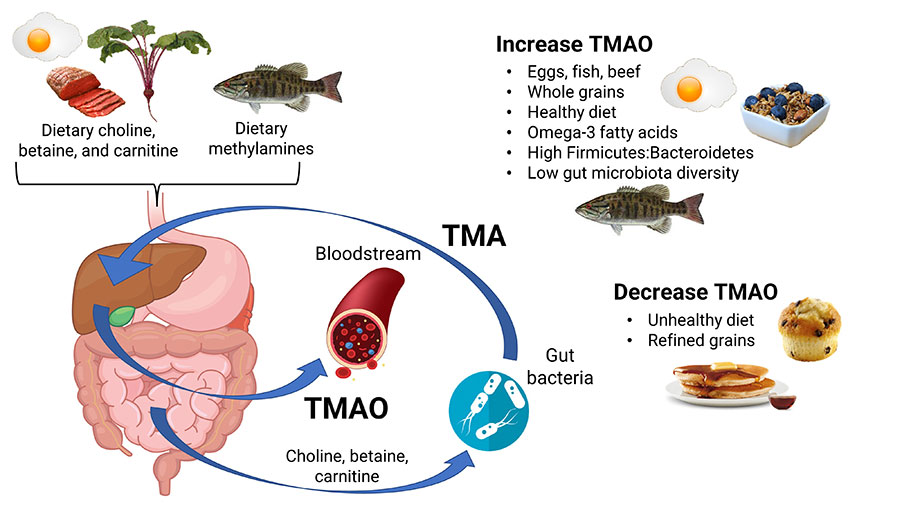
The collection of microbes (such as bacteria and viruses) that reside in the gastrointestinal tract, referred to as the gut microbiota, is important in overall human health and disease.76 Unhealthy changes in the gut microbiota have been linked to the development of atherosclerosis. Alterations of the gut microbiota can lead to increased permeability of the gut’s barrier to the bloodstream, allowing components such as lipopolysaccharide to enter the blood. Lipopolysaccharide can stimulate an inflammatory response that promotes atherosclerosis.77 An unhealthy microbiota itself can also produce deleterious metabolites that can trigger or worsen atherosclerosis. Research continues to evaluate whether and how manipulating the microbiota could modify cardiovascular risk. However, several studies suggest supplementation with Lactobacillus reuteri 30242 may support cardiovascular health.78-82 For more information, see Life Extension’s protocol on Maintaining a Healthy Microbiome.
Hormones and Cardiovascular Risk
Hormones are chemical messengers that serve critical roles in cellular communication throughout the body and help regulate various aspects of physiology and behavior. Maintaining a healthy balance among hormones, including progesterone, estrogen, dehydroepiandrosterone (DHEA), testosterone, and pregnenolone, is important for overall health.83 Hormone levels naturally decline as we age,83,84 and research suggests declining hormone levels may play a role in cardiovascular disease risk.
Hormonal health and CVD risk among men. Testosterone, the major male sex hormone, plays a role in sperm production, libido, and bone and muscle strength. Testosterone levels are at their highest in adolescence and early adulthood, and then they begin to gradually decline by the age of about 25.85 Low testosterone levels are associated with brittle bones, decreased libido, and irritability and depression.86 Life Extension suggests an optimal target level of free testosterone of 20‒25 pg/mL for most men.
Research suggests that low levels of testosterone are associated with an increase in all-cause mortality and cardiovascular risk, metabolic syndrome, and diabetes.87 Low levels of testosterone in men with coronary artery disease is associated with a poor prognosis.87 Testosterone replacement therapy has been shown to improve ischemia in men with coronary artery disease and improve exercise capacity in men with congestive heart failure.87
A recent meta-analysis examined the relationship between testosterone and cardiovascular risk in men. In all, 108 studies were examined, including randomized trials and epidemiological studies. The authors concluded that testosterone therapy reduced overall morbidity and mortality, particularly in obese patients.88 Another review concluded that low testosterone levels are a cardio-metabolic risk factor.89 A longitudinal follow-up study of 930 men with coronary disease found that testosterone deficiency was common and negatively affected survival.90 Other research in 79 males aged 33‒68 found that free and total serum testosterone levels are lower in men with acute myocardial infarction.91
While testosterone levels are important for a man’s overall health and well-being, other hormones, including DHEA, also play a role. DHEA is a steroid hormone that is metabolized into testosterone and estrogen. However, DHEA has many important functions in its own right. Some studies have suggested that DHEA supplementation supports cognitive function, energy levels, and a healthy body weight. A prospective population-based study in over 2,000 elderly men found that low levels of DHEA were predictive of the five-year risk of coronary heart disease.92 Life Extension suggests an optimal target level of DHEA-sulfate (DHEA-s) of 350‒500 µg/dL for men (and 275‒400 µg/dL for women).
A prominent study published in 2017 raised concerns about testosterone therapy and increased progression of coronary artery non-calcified plaque.93 However, a follow-up analysis published in late 2019 suggested that waist-to-hip ratio may modify the association between testosterone therapy and coronary plaque progression. The 2019 analysis found that as participants’ waist-to-hip ratio increased, so did coronary artery plaque progression among men assigned to testosterone therapy.94 More studies are needed to determine whether testosterone replacement therapy modifies coronary artery plaque progression in otherwise healthy men with a healthy waist-to-hip ratio.
Estrogen, the primary female sex hormone, also modulates sperm production and male libido. Although the role of estrogen in maintaining healthy bone mass in women is well known, men may not realize that estrogen plays an important role in maintaining bone health in males as well.95 Some evidence suggests keeping estrogen levels in a healthy range may benefit men’s cardiovascular health. In a prospective observational study involving 501 men with chronic heart failure, men with the highest and lowest amounts of estradiol had the highest mortality, while those in the middle group (with estradiol levels of 21.80‒30.11 pg/mL) had the fewest deaths. The researchers concluded that balanced estradiol levels are cardioprotective, perhaps due to protective effects of the heart tissue and vascular system.96 In another prospective cohort study of over 2,000 healthy middle-aged men, higher serum estradiol levels were associated with a lower risk of cardiovascular disease in older, but not younger, men.97 Life Extension suggests most aging men target an optimal estradiol blood level of 20‒30 pg/mL. Estradiol levels should be balanced with testosterone levels in men, and a healthy ratio of total testosterone to estradiol may be roughly 23:1 to 40:1.
More information is available in Life Extension’s Male Hormone Restoration protocol.
Hormonal health and CVD risk among women. The main sex hormones that guide female sexual function and reproduction are estrogen and progesterone. Declining hormone levels with menopause have been associated with several health conditions. Although the risks and benefits of hormone replacement therapy have been extensively debated, current evidence suggests initiating hormone replacement therapy near menopause offers cardiovascular benefits and minimal risks.98-100
In a large prospective cohort study of over 4,200 post-menopausal women, hormone replacement therapy was associate with lower all-cause mortality and less coronary atherosclerosis.101 In an open-label, randomized, controlled trial, over 1,000 women aged 45‒58 who were post-menopausal or had peri-menopausal symptoms were randomized to receive hormone replacement therapy or no treatment. After 10 years of intervention, the women receiving hormone therapy had significantly reduced risk of mortality, heart failure, and myocardial infarction, without an increased risk of cancer or stroke.102 Another study involving over 2,800 post-menopausal women found that higher estradiol levels were associated with a lower risk of cardiovascular disease.103
It is important for all aging individuals to monitor their hormone status. Comprehensive testing as well as regular physical examination by a doctor may help detect hormonal imbalances in aging individuals. Natural products including phytosterols may help promote healthy hormonal signaling. Bioidentical hormone replacement therapy, which uses hormones identical to those naturally made in the body, is the preferred method of hormone replacement therapy. Today, several FDA-approved bioidentical hormone replacement preparations are available.
More information is available in Life Extension’s Female Hormone Restoration protocol.
Nitric Oxide Deficit
Nitric oxide (NO) is a compound in the body that plays a role in cell signaling and helps facilitate healthy blood flow by promoting blood vessel relaxation. NO supports healthy arterial walls and allows arteries to maintain their elasticity. Age-related declines in NO may contribute to cardiovascular disease.104-106 Commercial blood tests for measuring NO levels in the body are currently not widely available.
Statin drugs may promote NO synthesis and can be taken at low doses with supplemental CoQ10.107,108 In addition, there are some dietary supplements that may help promote healthy NO levels. Arginine, an amino acid, is a precursor to the production of NO in the endothelium, and pomegranate also supports healthy NO synthesis and endothelial function.109,110
Elevated Homocysteine
Homocysteine is an amino acid present throughout the body. Excess homocysteine levels are implicated in atherosclerosis, through promotion of blood clotting factors and damage to the arterial lining.111 Many factors can contribute to elevated homocysteine levels, including insufficient intake of B vitamins, excess alcohol consumption, certain medications, and genetic variations that lead to inefficient folate metabolism. Life Extension recommends that homocysteine blood levels be kept below 8 µmol/L.
Elevated homocysteine levels can be lowered by medications such as Cerefolin. Natural therapies include supplementation with B vitamins, including methylfolate, vitamin B12, and vitamin B6, as well as trimethylglycine and N-acetylcysteine.112-114 Limiting alcohol consumption and consuming a diet low in meats (including beef, pork, chicken, and turkey) and high in fruits and vegetables and monounsaturated fats may also promote healthy homocysteine levels.
Refer to Life Extension’s Homocysteine Reduction protocol for more information.
Low EPA/DHA
Eicosapentaenoic acid (EPA) and docosahexaenoic (DHA) are omega-3 fatty acids that promote healthy neural development, vision, cognitive function, cardiovascular health, and inflammatory response. The FDA announced in mid-2019 that EPA/DHA supplements can make the qualified health claim that they may reduce the risk of hypertension and coronary heart disease; although the agency described the evidence available at the time as “inconclusive.”115 Research suggests omega-3 fatty acids reduce inflammation and modulate blood clotting and may help prevent peripheral artery disease and major coronary events.116
It has long been noted that higher intakes and blood levels of omega-3 fatty acids (relative to omega-6 fatty acids) are associated with cardiovascular health, including lower rates of heart attack. Evidence suggests an ideal omega-6 to omega-3 ratio is less than 4:1. The best ways to enhance levels of EPA and DHA are through quality fish oil supplements and a diet that includes cold water fish at least twice a week. This includes mackerel, lake trout, sardines, tuna, sea bass, and salmon.116
Low Vitamin D
Vitamin D supports bone health and may help reduce the risk of some forms of cancer. It also promotes cardiovascular health by reducing chronic inflammation and promoting healthy vascular cell function.117,118 Life Extension suggests a target level of vitamin D between 50 and 80 ng/mL of 25-hydroxyvitamin D for most people, and blood levels should determine the necessary supplemental dosage, which is typically between 1,000 and 7,000 IU daily. Vitamin D is also synthesized by the skin in response to sunlight exposure, although excessive sun exposure is a major risk factor for skin cancer.
Inadequate Vitamin K Intake
Vitamin K is a fat-soluble family of vitamin compounds that play a role in blood clotting and bone metabolism. It is naturally found in leafy green vegetables.119 Importantly, adequate vitamin K intake is critical for helping maintain healthy calcium balance in the arteries and bones. In fact, the older anti-coagulant drug warfarin blocks the activity of vitamin K and is associated with increased vascular calcification.120 Conversely, vitamin K supplementation (especially K2 supplementation) slows the progression of coronary artery calcification in people with pre-existing coronary calcification and helps improve vascular stiffness.121-123
While there is no defined optimal blood level for vitamin K, vitamin K supplements containing both K1 and K2 (as MK-4, MK-6, MK-7, and MK-9) can help ensure healthy vitamin K intake.
Elevated Fibrinogen
Fibrinogen is a protein found in the blood that plays an important role in blood clotting. Excess fibrinogen is associated with vascular disease via its effects on blood viscosity and cellular adhesion in the arteries.124,125 Life Extension suggests a target blood level of 295–369 mg/dL for fibrinogen.
Some prescription medications, such as statins, may lower fibrinogen levels. In addition, supplements such as fish oil, vitamin C, and Nattokinase may help promote healthy fibrinogen levels.126-128
Elevated C-reactive Protein (CRP)
C-reactive protein (CRP) is a nonspecific blood marker that connotes inflammatory status in the body.9 It is produced in many cells in the body, but CRP produced by fat and liver cells increases the production of cell adhesion molecules and plasminogen activator inhibitor-1, a protein involved in blood clotting. CRP also inhibits an enzyme that produces NO.28,129
Life Extension’s suggested target blood levels of CRP are less than 0.55 mg/L for men and less than 1.0 mg/L for women. Statin drugs have anti-inflammatory properties and can lower CRP levels.130,131 Dietary supplements such as vitamin C, curcumin, fish oil, borage oil, and Irvingia gabonensis extract may also reduce CRP or suppress inflammation.132-136 Consuming soluble fibers may also reduce inflammation and lower CRP levels.137 Weight loss, through a healthful diet (eg, the Mediterranean diet) and increased physical activity, reduces inflammation. In addition, avoiding foods cooked at high temperatures may reduce inflammation and levels of CRP in the body by reducing exposure to advanced glycation end products (AGEs).138
Apolipoprotein E (ApoE) Risk Variants
Apolipoprotein E (ApoE) is a protein that plays a role in fat metabolism. There are three genetic variants of ApoE, and they exert differential influence on cardiovascular risk. ApoE2 is associated with lower risk under most circumstances and ApoE4 is associated with higher risk, whereas ApoE3 is considered roughly neutral. ApoE4 also increases risk of Alzheimer disease.139,140 ApoE2 exerts its protective effects by helping the liver clear harmful lipoproteins from the body more effectively than the E3 and E4 variants.141-143 However, among people with hyperlipoproteinemia, ApoE2 may be associated with increased cardiovascular risk.
Elevated Serum Amyloid A (SAA)
Serum amyloid A (SAA) is a group of proteins produced by the liver in response to infection, inflammation, or injury.144 Because SAA blood levels are often increased in those with atherosclerosis, blood measurements have been used to identify those with or at risk of developing the disease.145 There is now evidence that SAA proteins play a direct role in the development and progression of atherosclerosis.146,147 SAA can stimulate macrophages to secrete inflammatory biochemicals and cell adhesion molecules, and modify HDL, reducing its protective effects.148
Elevated Tumor Necrosis Factor-alpha (TNF-α)
Tumor necrosis factor-alpha (TNF-α) is an inflammatory cytokine that plays a role in the initiation and progression of atherosclerosis. Specifically, TNF-α promotes the production of inflammatory factors, leads to the overproduction of cell adhesion molecules, and depresses levels of NO. TNF-α also causes direct harm to blood vessel linings by accelerating cell death.28 Natural compounds that may promote healthy levels of this biomarker include curcumin and resveratrol.149,150
Elevated Resistin
Resistin is a peptide-hormone that is not completely understood, but is thought to play a role in insulin tolerance or resistance.151,152 Macrophages found in atherosclerotic plaque produce resistin, where it is believed to contribute to the formation of foam cells, increase the production of cell adhesion molecules, and cause endothelial dysfunction. Increased resistin levels are found in cases of heart attack and near heart attack, and it is likely released into the blood during plaque rupture.153
While an optimal healthy range for resistin is not known at this time, preliminary research suggests vitamin C and garlic may help reduce resistin levels.154,155
Elevated Leptin
Leptin is a hormone that regulates hunger. Normally, leptin inhibits hunger, but abnormally elevated levels can lead to the body becoming resistant to its effects, which promotes overeating and obesity. In atherosclerosis, leptin excess contributes to endothelial dysfunction, inflammation, and oxidative stress.156 Furthermore, irrespective of its role in inflammation, leptin can promote thrombosis.28
Leptin levels vary day to day and typically decline with age, and leptin is higher in women than in men. In one study, fasting leptin levels above 15 ng/mL were associated with insulin sensitivity issues,157 and in another study values above 23.75 ng/mL in women and 6.45 ng/mL in men were associated with cardio-metabolic abnormalities.158 While research is ongoing, a diet rich in monounsaturated fatty acids and low in excess fat, cholesterol, and calories is believed to support healthy leptin levels.159 In addition, 10 weeks of supplementation with Irvingia gabonensis extract has been shown to reduce leptin levels in overweight subjects.132
Elevated Lipoprotein (a)
Lipoprotein (a), also called Lp(a), is a subclass of lipoprotein particles composed of LDL-like particles bound to another particle, called apolipoprotein(a). Lp(a) is a known marker of cardiovascular risk; that is, elevated levels correlate with greater risk for cardiovascular disease. Lp(a) levels are mostly determined by genetics (as opposed to diet and lifestyle as with other blood lipid markers). Generally, Lp(a) levels above 50 mg/dL (~125 nmol/L) are considered to indicate high cardiovascular risk, whereas levels below 30 mg/dL (~72 nmol/L) are associated with low risk.160
Lp(a) levels should be interpreted in the context of other cardiovascular and lipid risk markers, and family history of cardiovascular disease is an indication for measurement of Lp(a). As of mid-2019, no reliable data from randomized controlled trials have shown that targeting Lp(a) reduction with medication is an effective risk-reduction strategy. As of this writing, the only intervention available that appears promising for lowering Lp(a) is lipoprotein apheresis.161 Lipoprotein apheresis involves the removal of lipoproteins from the blood via a blood filtration process used only in people with very elevated blood lipids despite maximal lifestyle and drug therapy. Thus, Lp(a) is primarily useful as a marker for identifying people who might benefit from adopting a more intensive overall cardiovascular risk reduction strategy.
Nevertheless, some intriguing interventions that target Lp(a), such as antisense oligonucleotides, are currently under development and may represent a novel intervention if research progresses as hoped, but further studies are needed.162-165
6 Atherosclerosis Prevention
In most cases, atherosclerosis is preventable because many factors that contribute to its development are modifiable. Assessing your risk and making appropriate dietary and lifestyle changes are key. This section outlines several considerations that can help you understand your risk of cardiovascular disease and the steps you can take to reduce it.
Atherosclerosis is a complex and multifactorial process. Please see Life Extension’s protocols on Cholesterol Management, High Blood Pressure, Homocysteine Reduction, Stroke, and Diabetes and Glucose Control for more information on cardiovascular health and disease prevention.
Adopt a Healthy Diet
A healthy diet contains plenty of vegetables, fruits, nuts, whole grains, and fish, and less processed foods, red meats, refined carbohydrates, and sweetened beverages. In addition, a diet rich in pro-inflammatory omega-6 fatty acids and deficient in anti-inflammatory omega-3 fatty acids promotes inflammation and oxidative stress, which has been linked to numerous age-related diseases.170,171
High-sodium diets have long been understood to contribute to hypertension and adverse cardiovascular outcomes. In a 2021 meta-analysis of 85 clinical trials, changes in dietary sodium intake and the impact on blood pressure was measured. Sodium intake in the various studies ranged from 0.4 to 7.6 grams per day and consistently showed a linear association with blood pressure. Participants with and without hypertension showed a decrease in blood pressure with sodium reduction; a 2.3 gram per day decrease in sodium intake was associated with a 2.30 mm Hg reduction in systolic blood pressure and 0.80 mm Hg average lower diastolic blood pressure in those without hypertension. This association was stronger in those with hypertension and resulted in a 6.50 mm Hg and 3.00 mm Hg reduction in average systolic and diastolic blood pressure, respectively.419
The balance between sodium and potassium appears to have a strong impact on cardiovascular health as well. In an analysis of six prospective cohort studies that included nearly 11,000 participants, higher sodium and lower potassium intake was associated with increased cardiovascular risk. Sodium and potassium intake were measured in multiple 24-hour urine samples. Each daily increment of 1,000 mg sodium excretion was associated with an 18% increased risk of coronary revascularization, myocardial infarction, or stroke, while each daily increment of 1,000 mg potassium excretion was associated with an 18% decreased risk. Additionally, individuals in the quartile with the highest sodium-to-potassium ratio had a 62% increased cardiovascular risk compared with those in the lowest quartile.420 And in a large open-label trial that included over 20,000 participants in rural China, most of whom were over 60 years old and had a history of stroke and hypertension, substitution of regular sodium salt with a salt containing 25% potassium chloride significantly reduced the rates of stroke, major cardiovascular events, and mortality.421
A large meta-analysis that examined over 45 prospective studies determined that there is a large, strong, and consistent body of evidence to support the benefits of the Mediterranean Diet on cardiovascular health.172 The Mediterranean diet has consistently been shown to reduce the risk of atherosclerotic cardiovascular disease. This diet, which is low in animal products and saturated fat, and high in olive oil, legumes, fruit, vegetables, and fish has been shown to reduce the risk of heart attack, stroke, and dying from cardiovascular disease by about 30%.173
In a recent prospective cohort study of nearly 26,000 women in the United States, those with the highest intake of Mediterranean foods had a 28% reduction in risk of cardiovascular events. This was mostly attributed to reduced biomarkers of inflammation, glucose metabolism, insulin resistance, and adiposity.174
A pesco-Mediterranean diet is similar to the traditional Mediterranean diet, but with an emphasis on consuming fish or seafood at least three times per week, limiting intake of fresh red and white meat, and removing all processed meats from the diet. In the pesco-Mediterranean diet, seafood is the predominant source of animal protein, providing omega-3 fatty acids along with zinc, iodine, selenium, B vitamins, calcium, and magnesium. Although there is currently no evidence for adverse outcomes associated with high levels of fish consumption, low-mercury fish (eg, salmon, sardines, or trout) should be eaten when possible.379 The seafood component of the pesco-Mediterranean diet may offer benefit over a solely plant-based diet. In a study of more than 48,000 people, pesco-vegetarians (consumers of seafood as the primary source of animal protein) had a 13% lower risk of ischemic heart disease than meat eaters. Vegetarians (who reported eating no meat or fish, but did report consuming dairy or eggs), had a 22% lower risk of ischemic heart disease, but also a higher risk of stroke than meat eaters.380
Some experts suggest combining the pesco-Mediterranean diet with time-restricted eating may be an optimal diet for heart health. Time-restricted eating, which is a form of intermittent fasting, typically limits food intake to a 6- to 10-hour window during the active phase of the day.381,382 After an overnight fast of at least 12 hours, insulin levels are lowered and carbohydrate stores are depleted. At this point, fatty acids from fat tissue are metabolized instead of sugars, which can improve insulin sensitivity. Several preliminary studies have suggested that time-restricted eating offers some cardiometabolic benefits, particularly for obese individuals.379,383,384 However, rigorous studies on the benefits of intermittent fasting are uncommon, and a randomized clinical trial published in September 2020 failed to show benefits in overweight and obese individuals.385 More studies on the effects of intermittent fasting are needed.
Research indicates that the ideal dietary ratio of omega-6:omega-3 fatty acids is 4:1; however, the typical Western diet has a ratio of 20:1.175 Most people have a diet deficient in omega-3s and too high in omega-6s as compared to the diet that humans evolved with.176 This change in dietary composition parallels the rise in overweight and obesity in Western society.177 Elevated levels of omega-6 polyunsaturated fatty acids and higher omega-6:omega-3 ratios promote many chronic diseases, including cardiovascular disease, cancer, asthma, and autoimmune disease.176
Be Physically Active
American adults average six to eight hours a day sitting, despite the well-known association between sedentarism and an increased chance of developing and dying from cardiovascular disease.178 Regular physical activity has been shown to be beneficial in those with atherosclerosis. Formal protocols called cardiac rehabilitation, supervised by medical practitioners either in a medical practice or at home, are encouraged, but do-it-yourself programs are also beneficial.
The American Heart Association recommends at least 150 minutes per week of moderate-intensity activity or 75 minutes of vigorous-intensity activity. Moderate intensity activities include brisk walking, biking at a speed of 5‒9 miles per hour, dancing, active yoga, recreational swimming, or any activity that puts one near, but not past, the point of being unable to speak a complete sentence without pausing for breath.179 Examples of vigorous activities are jogging, biking at speeds greater than 10 miles per hour, resistance training, and swimming laps. Resistance training includes muscle-strengthening tasks such as weightlifting or the use of elastic bands or one’s own body weight to improve body strength. In some cases, this type of activity improves lipid profiles beyond what aerobic activity alone can.179,180 In addition to a physical activity program, individuals should combat a sedentary lifestyle by increasing daily physical activity by keeping busy with household work, gardening, and taking the stairs instead of elevators, etc.
A 2021 study in 305 participants with peripheral arterial disease found high-intensity walking, defined as a pace that elicited ischemic leg pain, five times per week for one year increased 6-minute walking distance by an average of 35 meters. By contrast, those assigned to low-intensity walking exercise or no exercise did not experience improved 6-minute walking distance.387 The authors of the study concluded that patients with peripheral arterial disease should “walk for exercise at a pace that induces ischemic leg symptoms in order to get a benefit.”
For more information, see the section titled “Lack of Physical Activity.”
Sleep
Sleep has a vital and complex effect on overall health, including cardiovascular health and function, and ultimately influencing the risk of death from cardiovascular or any cause.422-426 A growing body of evidence for this relationship is reflected in the 2022 Presidential Advisory from the American Heart Association that updates their “Life’s Essential 7” (now 8) to include sleep as a critical and consensus variable for heart health.423
Much sleep research has examined the role of sleep duration in promoting optimal health at various ages and for different health outcomes.427 There is general agreement that 7-9 hours of sleep per night is recommended for adults.428,429 While an adequate but not excessive amount of sleep is beneficial for cardiovascular and other aspects of health, duration is not the only contributor to sleep quality.425,430
Other important components of quality restorative sleep include sleep consistency or regularity; timing, meaning early or late bedtime and wakeup; and fragmentation or interruption of sleep.427,431 Sleep fragmentation refers to a loss of sleep quality due to interruptions from various causes.
The cardiovascular system is powerfully influenced by circadian rhythms—the wake/sleep, day/night, light/dark cycle. Irregular sleep schedules that result in variable sleep duration and timing have the potential to disrupt circadian rhythms. An observational study published in 2020 reported on 1,992 participants from the Multi-Ethnic Study of Atherosclerosis who went through a seven-day sleep evaluation from 2010 to 2013 and were then followed-up through 2016. The researchers found that, over the nearly 5-year follow-up period, participants with the most irregular sleep duration or timing were more than twice as likely to develop cardiovascular disease compared with those with the most regular sleep patterns.432
Another study assessed the relationship of both sleep duration and sleep quality with atherosclerosis in 3,974 participants from a Spanish prospective cohort study called Progression of Early Subclinical Atherosclerosis. After adjusting for an array of risk factors, the investigators found ultrasound evidence that participants who got less than six hours of sleep per night were more likely to have higher non-coronary plaque burden, compared to those who got seven to eight hours of sleep per night. A separate analysis found that those with the most sleep fragmentation were significantly more likely to have multiple regions of noncoronary atherosclerotic plaque, compared to those with the least sleep fragmentation.433
One of the major causes of sleep fragmentation is obstructive sleep apnea, which is increasingly recognized as an influential cardiovascular risk factor.434,435 A study in 1,465 participants from the Multi-Ethnic Study of Atherosclerosis found that both obstructive sleep apnea severity as well as increased sleep interruptions raised the risk of coronary artery calcification.436 Among 4,887 subjects enrolled in the Sleep Heart Health Study, participants with greater sleep fragmentation and normal blood pressure had an elevated risk of congestive heart failure over a 10-year follow-up period.431
Sleep hygiene is an umbrella term for healthy sleep habits that encourage proper and restful sleep.437,438 Though there have not been controlled sleep hygiene intervention trials in cardiovascular diseases, sleep and lifestyle habits that encourage restful, restorative sleep are important for everyone, including those concerned with heart disease prevention and management.439
Avoid Tobacco Use and Second-hand Exposure
Tobacco use is a major modifiable risk factor for many diseases, including cardiovascular diseases such as coronary artery disease, stroke, vascular disease, congestive heart failure, angina, and aortic aneurysms. Smoking cigarettes is a causative factor in approximately one in five deaths in the United States each year.181 It is known to damage the heart and blood vessels, and elevates cholesterol and blood pressure levels. It also prevents oxygen from adequately reaching all of the body’s organs and tissues.27 Research suggests cigarette smoke causes oxidative stress, vascular dysfunction and inflammation, platelet coagulation, and impairs the serum lipid profile in both active and passive smokers.
Those who use tobacco should strongly consider quitting. The process of quitting can be different for each person and should be individualized; however, successful quitting most often involves a combination of tobacco cessation counseling and nicotine replacement. Any level of exposure to tobacco smoke is harmful. Nonsmokers who are regularly exposed to second-hand smoke are at risk of developing cardiovascular disease and stroke,182 and even a brief encounter with smoke may be harmful.183
Limit Alcohol Intake
There is some evidence that light drinking may be heart-healthy. However, the evidence is relatively weak as it is based on observational studies and not controlled trials. It is not generally recommended to start drinking alcohol for any perceived benefit on atherosclerosis.5 For those who do partake, light drinking should be emphasized, limiting consumption to one drink (four ounces of wine or one ounce of liquor) per day for women and no more than two drinks per day for men.
Consider Medication to Lower Cholesterol
People with a very high LDL (greater than or equal to 190 mg/dL), diabetes, those between 40‒75 years of age, and those who have an elevated risk through cardiovascular risk estimation may require more aggressive cholesterol lowering strategies, including medication. Statins (eg, atorvastatin [Lipitor] and rosuvastatin [Crestor]) are the pharmaceuticals most often recommended for preventing cardiovascular disease. Statins inhibit the activity of HMG-CoA reductase, a key enzyme in cholesterol synthesis, and may also reduce CHD risk by other mechanisms, such as reducing inflammation.184
Reduction of total cholesterol and LDL cholesterol (and/or triglycerides) by drugs usually involves inhibiting cholesterol production in the body or preventing the absorption/reabsorption of cholesterol from the gut. When the availability of cholesterol to cells is reduced, they are forced to pull cholesterol from the blood (which is contained in LDL particles). This has the net effect of lowering LDL cholesterol. Therapies that increase the breakdown of fatty acids in the liver or lower the amount of VLDL in the blood also result in lower serum cholesterol levels. Often, complementary strategies (eg, statin to lower cholesterol production plus a bile acid sequestrant to lower cholesterol absorption) are combined to meet cholesterol-lowering goals.
Consider Aspirin (For Those at High-risk)
Aspirin has long been used to prevent heart attacks in those at risk of cardiovascular events due to its role in preventing thrombosis, the underlying cause of heart attacks. Recent large-scale studies have helped redefine the groups of people most likely to benefit from aspirin therapy. The European Society of Cardiology does not recommend aspirin or aspirin-like therapy for individuals without established cardiovascular disease,185 and the American Heart Association states that daily, low-dose aspirin might be considered as a preventative measure among select adults 40 to 70 years of age who are at higher ASCVD risk but not at increased bleeding risk.186 Current evidence suggests aspirin is not helpful for primary prevention of cardiovascular events among people at low baseline cardiovascular risk.
The American Heart Association indicates that daily low-dose aspirin should not be used on a routine basis to prevent heart disease in those older than 70 years and not at all as a preventative in adults of any age who have a history of abnormal bleeding (eg, in the stomach or intestine); stomach or intestinal ulcers; low blood platelets; those who use medications that increase bleeding, such as anticoagulants or other blood thinners; and those with certain other medical conditions. In addition, aspirin therapy is not appropriate for those who drink alcohol on a regular basis.
Recent research has demonstrated an increased risk of major bleeding episodes, and recent trials have failed to show that aspirin was effective at preventing major cardiovascular events, including heart attack and stroke.187 An observational study tracked over 33,000 people with atherosclerosis and found that aspirin was only slightly beneficial for those with a history of heart attack or stroke, but not beneficial for those with no such medical history.188
In another trial, adults with diabetes (but no cardiovascular disease) randomly received either 100 mg of aspirin per day or placebo. More than 15,000 subjects were followed for over seven years, with the primary endpoints being serious vascular event (such as stroke, heart attack, or death from vascular causes) or major bleeding event, such as serious bleeding or hemorrhage. The researchers found that aspirin prevented vascular events in those with diabetes but no cardiovascular history, but also caused major bleeding events.189
In another randomized, double-blind, placebo-controlled, multicenter trial, over 12,000 men aged 55+ and women aged 60+ with an average cardiovascular risk received either 100 mg aspirin or placebo daily. Researchers were not able to conclude that aspirin was more effective than placebo at preventing a major cardiovascular event such as cardiovascular death, myocardial infarction, unstable angina, stroke, or transient ischemic attack.190 In yet another randomized placebo-controlled trial involving over 19,000 people aged 70 years and older who received 100 mg aspirin for five years to determine if aspirin had an impact on death, dementia, or physical disability, researchers concluded that aspirin use did not prolong disability-free survival and led to a higher rate of major hemorrhage as compared with placebo.191
Do not take daily low-dose aspirin without the guidance of a physician, as the risk and benefits vary with each person. Aspirin can be used as part of a treatment plan for a person who has a history of stroke or heart attack. Follow only the treatment plan that your physician has established for you.
Four Heart Health Myths
7 Atherosclerosis Treatment
The American Heart Association provides atherosclerosis treatment guidelines to health care providers and their patients.5 These guidelines are intended to prevent fatalities from atherosclerosis, nonfatal heart attacks, and damage to heart function, which could lead to heart failure.
As noted earlier, atherosclerosis is a complex and multifactorial process. Please see Life Extension’s protocols on Cholesterol Management, High Blood Pressure, Homocysteine Reduction, Stroke, and Diabetes and Glucose Control for more information on cardiovascular health and disease treatment.
One cornerstone of therapy for atherosclerosis is managing the underlying conditions that lead to its onset and progression (risk factor modification). This section summarizes several key targets for modification. In addition, Life Extension encourages people who wish to promote optimal cardiovascular health to take steps to manage all the risk factors described earlier in this protocol.
Managing Blood Lipids
A multifaceted approach is recommended to modify blood lipids. This includes lifestyle elements, nutritional supplements, and pharmaceutical treatment. Daily physical activity is advised, and weight loss is encouraged, as a 10-pound weight loss is associated with a lowering of LDL by 5‒8%.192 Intake of saturated fats should be limited to less than 7% of total calories and trans-fats should be avoided. Supplementation of plant stanols/sterols and viscous fiber have also been shown to reduce LDL.
Current guidelines generally recommend high-dose statin medications for most people with atherosclerosis, unless there are contraindications or intolerable side effects.51
For individuals with atherosclerosis who are identified as being at high risk, Life Extension recommends that the LDL level be kept below 70 mg/dL. This applies to those with multiple cardiovascular disease events or one cardiovascular event and multiple high-risk characteristics.51 Cardiovascular events include heart attack, near heart attack within the past 12 months, stroke due to plaque rupture, or any symptomatic peripheral atherosclerosis. High-risk characteristics include age older than 64 years, diabetes, high blood pressure, chronic kidney failure, current smoking, and heart failure, among others. If this goal cannot be reached with statins alone, then ezetimibe (Zetia) may be added to the medication regimen, followed by a PCSK9 inhibitor.
Managing Blood Pressure
In those who have atherosclerosis and high blood pressure, blood pressure control is paramount. Lifestyle modification alone can be attempted first to see if blood pressure can be controlled without medication. This involves weight control, increased physical activity, and a diet low in sodium with lots of fresh fruits, vegetables, and low-fat dairy products. However, medication is often needed as well.
The blood pressure treatment target may vary depending on the patient’s established risk factors and overall baseline risk. Life Extension’s High Blood Pressure protocol contains information about managing blood pressure effectively using lifestyle, diet, pharmaceuticals, and integrative interventions. Because different blood pressure treatment targets may be appropriate for different patients, you should consult with your physician before implementing a blood-pressure-lowering medication regimen.
A review of studies examining aerobic exercise found that regular moderate-intensity exercise can lower systolic blood pressure by about 3.84 mm Hg and diastolic blood pressure by 2.58 mm Hg.193 In people who are overweight, even modest weight loss (4‒8% of body weight) can lead to a 3 mm Hg drop in systolic and diastolic blood pressure.194 A review of studies that focused on the effects of excessive alcohol consumption on high blood pressure found that quitting drinking or limiting alcohol to one or two drinks per day resulted in a 3.3 mm Hg reduction in systolic blood pressure and a 2 mm Hg reduction in diastolic blood pressure.195 Reducing sodium intake can lower systolic blood pressure by 3.39 mm Hg and diastolic blood pressure by 1.54 mm Hg.196 A very effective lifestyle modification appears to be the DASH-sodium diet, which combines a reduced sodium diet with one that emphasizes vegetables, fruits, and low-fat dairy products. In one clinical trial, compared to participants in a higher sodium diet group, hypertensive participants in the DASH-sodium group experienced a reduction of 20.7 mm Hg for systolic blood pressure and 7.9 mm Hg for diastolic blood pressure.197
If a medication is needed to achieve the goal, then the most common pharmaceuticals employed are thiazide diuretics (hydrochlorothiazide, chlorthalidone, and others), beta blockers (metoprolol [Lopressor, Toprol XL], atenolol [Tenormin], and others), and ACE inhibitors (lisinopril, captopril, and others) or angiotensin receptor blockers (ARBs) (eg, telmisartan [Micardis]). Certain medications are preferred under certain conditions. For example, beta blockers are favored in those who have had a heart attack, and ACE inhibitors are the preferred treatment in individuals who have both high blood pressure and diabetes. Life Extension Magazine published a 2015 article on ancillary benefits of the ARB telmisartan, which may be a good choice for initial treatment in appropriately selected patients.
Managing Diabetes
In the context of atherosclerosis and cardiovascular disease, the official position of the American Heart Association on hemoglobin A1c (HbA1c) is that a goal of 7% or less is “reasonable” for certain patients, like “those with a short duration of diabetes mellitus and a long life expectancy.”5 However, because clinical studies have failed to show a clear advantage for intensive glucose control on cardiovascular events, the recommendations also state that a goal between 7% and 8% is reasonable in other instances, such as advanced age or a history of low blood sugar.
The main noninsulin agent used in the treatment of diabetes, metformin, has been shown to reduce the incidence of heart attack.198 Two or more medications are often necessary for optimal treatment, and not all medications are created equal in terms of cardiovascular risk. For example, rosiglitazone (Avandia), a member of a commonly-used class of medications called thiazolidinediones, has been associated with an increase in cardiovascular risk.5 Since the development of thiazolidinediones, two newer classes of medications for diabetes with clear cardiovascular benefits have been introduced.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors block the kidneys’ ability to bring glucose back into the blood after filtering it, which leads to increased excretion of glucose into urine. A clinical trial looking at the cardiovascular effects of the SGLT2 inhibitor empagliflozin in patients with type 2 diabetes demonstrated a reduction in death from cardiovascular causes and nonfatal heart attack and stroke.199 This benefit has been shown to extend to another medication in this class, canagliflozin.200
Glucagon-like peptide-1 (GLP-1) analogues are injectable medications that are useful in the treatment of diabetes because they stimulate the release of natural insulin. Notably, two members of this class of medications have been shown to reduce cardiovascular disease event rates, liraglutide 201 and semaglutide.202
Physical Activity
Regular physical activity has been shown to be beneficial in those with atherosclerosis. For more information on cardiovascular health and physical activity, please see the “Lack of Physical Activity” and “Be Physically Active” sections earlier in the protocol.
Body Weight
Body weight, body mass index (BMI), and/or waist circumference are often recorded as vital signs, along with blood pressure and pulse rate, at each health care provider visit. The goals from the American Heart Association are a BMI between 18.5 and 24.9 kg/m2 and a waist circumference less than 40 inches in men and 35 inches in women. Because even modest weight loss improves risk factors for atherosclerosis, for those for whom weight loss is advised, an initial goal of 5‒10% loss of body weight is appropriate.194
Previously many health care providers believed the so-called obesity paradox, which is the belief that being overweight or obese had a protective effect on certain cardiovascular risk parameters. This notion was originally supported by some scientific evidence, but subsequent large studies, including one published in the Journal of the American Medical Association in 2018, cast overwhelming doubt.203 The JAMA study, which pooled data from 10 separate studies involving nearly 200,000 patient encounters over 50 years, concluded that being obese (BMI of 30‒39.9) was associated with a shorter lifespan and a definite increase in cardiovascular disease incidence and death from cardiovascular disease. Those who were overweight (with a BMI of 25‒29.9) had a definite increased risk of cardiovascular disease compared to the group with a BMI of 18.5‒24.9.
Additional Medical Therapy
In 2014, the American Heart Association revised their guideline regarding two additional therapies.204
Chelation therapy. Chelation therapy refers to an intravenous infusion of a compound called disodium ethylenediamine tetraacetic acid (EDTA), which chelates or binds certain blood electrolytes, like calcium and cadmium. Once advocated by some to be helpful in the treatment of atherosclerosis, the promise of benefit was subsequently debunked by controlled studies. However, the thinking on chelation therapy has evolved again. In light of a new trial showing some benefit205 (but not enough to make a recommendation for its use), the American Heart Association said that the “usefulness of chelation therapy is uncertain” to reduce cardiovascular events in patients with stable ischemic heart disease.204 A large-scale randomized controlled trial to assess the benefits of chelation therapy plus a multivitamin in people with diabetes and a history of cardiovascular disease is underway as of the time of this writing (December 2019). The estimated completion date of the trial, called TACT2, is December 2022.
Enhanced external counterpulsation (EECP). EECP is a procedure that involves inflating pressure cuffs on the legs to aid lower extremity circulatory return. EECP was shown to improve cardiac output in a small study on eight patients with angina. The researchers speculated this effect may have arisen as a result of increased peripheral oxygen demand. EECP is typically administered over 35 treatment sessions spanning seven weeks, five days per week, for one hour per treatment session.206
EECP received FDA approval in 1995 for the treatment of angina pectoris when symptoms do not respond to most treatments. In 2014, the data was re-examined, and it was concluded that EECP may be considered for relief of refractory angina in patients with stable ischemic heart disease. The 2014 multi-society guidelines on the Management of Patients with Stable Ischemic Heart Disease concluded that most data were derived from small, heterogeneous studies, and more studies are needed to strengthen the recommendation for EECP.204
EECP has also been studied in the context of heart failure. The Prospective Evaluation of Enhanced External Counterpulsation in Congestive Heart Failure (PEECH) trial, published in 2006, found that EECP improved quality of life, NYHA functional classification, and exercise tolerance. However, in this study, EECP intervention satisfied only one of two pre-defined primary endpoints—it improved the percentage of subjects with a 60-second or more increase in exercise duration, but not VO2 max.207 In a randomized controlled trial published in 2015, EECP improved functional capacity significantly more than sham-EECP treatment among heart failure patients.208 Another study showed that EECP reduced myocardial oxygen demand by 19% in patients with left-ventricular dysfunction.209
EECP has also shown some potential for utility in other conditions in small, early studies as well. In a preliminary study, EECP was shown to be safe and feasible in patients with acute ischemic stroke, with minor improvements in blood flow velocity in the middle cerebral artery. The researchers called for further study.210 Intriguingly, EECP has also been shown to improve markers of glycemic control and glycation burden among diabetic patients, but this needs to be explored in additional studies.211,212
Because EECP is non-invasive and generally well tolerated, there is little downside to asking your health care provider whether EECP may benefit you. It will be important, however, to consider cost, as your insurance company may not cover EECP for conditions other than those for which it is FDA-approved.
Surgical Procedures and Interventions
In some cases, a more invasive atherosclerosis treatment plan may be advisable. For example, the best approach to the treatment of certain patients with atherosclerosis and ischemic heart diseases is to mechanically restore coronary artery blood flow with surgery or a catheter-based intervention.
With coronary artery bypass grafting (CABG) surgery, a heathy blood vessel from elsewhere in the body is stitched around a severe coronary artery plaque to bypass the plaque and restore blood circulation to the heart muscle. There are several variations to this surgery, but all involve significant risks and prolonged recovery periods.217
In a catheter-based intervention, the heart is accessed through a puncture in a wrist or groin artery to deliver a catheter to the coronary arteries. The inserted end of the catheter is equipped with a balloon, which is inflated in a procedure called angioplasty, thereby relieving a blood flow problem caused by significant coronary plaque. After removing the balloon, in most cases, a metallic stent is permanently implanted at the site of the angioplasty to prop open the artery and maintain blood flow.
These more invasive treatments are reserved for very severe and extensive coronary atherosclerosis because mechanical blood flow restoration has been shown to reduce the risk of death in these cases. In less severe cases, invasive treatments are employed if medications, lifestyle changes, and external procedures fail to adequately relieve chest pain, breathlessness, or fatigue that can be caused by ischemic heart disease.5
8 Nutrients
Consuming Ample Healthy Fatty Acids
Dietary fatty acids can be broadly categorized as saturated, monounsaturated, or polyunsaturated. The difference lies in variations in the chemical bonds between carbon and hydrogen atoms in the hydrocarbon backbone of the fatty acid molecule. Saturated fatty acids are relatively linear molecules. On the other hand, because of the effects of carbon-carbon double bonds, unsaturated fatty acids have bends or kinks in their fatty acid chain. Monounsaturated fatty acids (MUFAs) have one double bond, while polyunsaturated fatty acids (PUFAs) have two or more double bonds. Trans-fats are unsaturated fats, but have the linear configuration of saturated fats. Overall, dietary monounsaturated and polyunsaturated fatty acids are healthy, while saturated fats and trans-fats should be avoided.
The American Heart Association recommends consuming monounsaturated and polyunsaturated fats to replace saturated and trans-fats in the diet to improve lipid profiles and reduce cardiovascular risk.364,365
Monounsaturated fatty acids. Olive oil is a rich source of dietary MUFAs. Some other vegetable oils also contain abundant MUFAs; these include canola, peanut, soybean, sesame, and high-oleic safflower oils. However, extra-virgin olive oil (EVOO) may be the preferred oil-based source of MUFAs because it contains other healthy compounds aside from its MUFA content and has been linked to health benefits in many studies. Whole-food sources of MUFAs include almonds, cashews, peanuts, and avocados.366,459 The most-studied dietary MUFA source, with a vast body of evidence for benefit to cardiovascular and other aspects of health, is extra virgin olive oil. EVOO is a source not only of abundant MUFAs but also bioactive compounds including polyphenols, and is a superior source of polyphenols compared with other grades of olive oil and other culinary oils.367-369 EVOO and olive polyphenols exert a range of beneficial effects that can lower cardiovascular disease risk, including vasodilatory effects, anti-inflammatory activity, defense against oxidative stress, improved lipid profiles and HDL functionality, and even blood sugar control.370-373
A study published in mid-2020 examined the association between dietary olive oil intake in the United States and cardiovascular risk. The study followed over 92,000 subjects for up to 24 years. Those whose olive oil intake was greater than half a tablespoon daily had a lower risk of cardiovascular disease overall as well as a reduction in coronary heart disease specifically. Importantly, the study also found that replacing 5 grams per day of margarine, butter, dairy fat, or mayonnaise with an equivalent amount of olive oil was also associated with a lower cardiovascular disease risk.374 An earlier 4.8 year-long controlled clinical trial in close to 7,500 individuals at high risk of cardiovascular disease found a 31% reduced risk of major cardiovascular events in those following a Mediterranean diet supplemented with EVOO, compared to those on a control low-fat diet.375
Polyunsaturated fatty acids. Polyunsaturated fatty acids (PUFA) include omega-3 fatty acids found in seafood, fatty fish, fish oil, vegetable oils, and walnuts. As mentioned previously, the ideal dietary ratio of omega-6:omega-3 fatty acids is 4:1; however, the typical Western diet has a ratio of 20:1.175 Most people have a diet deficient in omega-3s and too high in omega-6s as compared to the diet that humans evolved with.176 This change in dietary composition parallels the rise in overweight and obesity in Western society.177 Elevated levels of omega-6 polyunsaturated fatty acids and higher omega-6:omega-3 ratios promote many chronic diseases, including cardiovascular disease.176
Three large controlled scientific studies have provided evidence that greater PUFA intake is associated with a reduction in the incidence of cardiovascular events in those with atherosclerosis.224-226 A 2019 meta-analysis found that greater omega-3 PUFA intake was associated with reduced cardiovascular risk in long-term studies that provided follow-up periods of 10 years. This finding suggests long-term, consistent intake of healthy PUFAs may be important for cardiovascular health.227
Regarding omega-3 supplementation in the context of cardiovascular outcomes, the controlled trials preformed to date have varied a great deal in their design and methods. Not surprisingly, study results and interpretations of the findings have been inconsistent. However, as of late 2019, the benefit of higher omega-3 dosages have become apparent. A meta-analysis published in the Journal of the American Heart Association pooled data from 13 randomized controlled trials involving nearly 130,000 participants. This analysis found a dose-response relationship between omega-3 supplementation and a reduction in risk of several cardiovascular outcomes. That is, higher doses of omega-3 supplementation were linked to greater risk reductions.228 A 2020 analysis evaluating the effect of omega-3 dosing on cardiovascular outcomes in a combined total of more than 135,000 participants showed supplementation with 400 to 5,500 mg/day of the omega-3 fatty acids EPA and DHA reduced the relative risk for fatal heart attack by 35%. Other cardiovascular benefits included a relative risk reduction of 13% for any heart attack, 10% for adverse events from coronary heart disease, and 9% for mortality from coronary heart disease. Furthermore, higher doses of omega-3 supplementation resulted in more cardiovascular protection. For every 1,000 mg/day increase in EPA/DHA intake (up to 5,500 mg/day), the relative risk of cardiovascular events and heart attack decreased by 5.8% and 9.0%, respectively.386
Other studies suggest omega-3 supplementation may be particularly useful in certain subgroups of people. For example, a controlled trial involving approximately 7,000 patients with heart failure found that omega-3 supplementation reduced risk of death or hospitalization due to cardiovascular causes.229 One trial demonstrated that fish oil supplementation reduced the risk of death in people who suffered a heart attack within the past three months.225 The American Heart Association recently declared that PUFA supplementation is reasonable to help prevent cardiac death in patients with prevalent coronary heart disease and to help prevent outcomes in those with heart failure.230
More recently, in a large multicenter trial (REDUCE-IT), over 8,000 patients with (or at risk for) atherosclerosis and elevated blood triglycerides were randomized to receive a highly purified prescription form of the omega-3 fatty acid eicosapentaenoic acid (EPA, as icosapent ethyl) or placebo. The icosapent ethyl group had a significant drop in risk of heart attack, stroke, and death from any cardiovascular cause.231 A post-hoc analysis further found that those in the icosapent ethyl group had a 34% reduction in first revascularization procedures and a 36% reduction in total revascularizations. In the icosapent ethyl group, stenting procedures were reduced by 32% and CABG dropped by 39%.376 Additionally, a review of 16 controlled human trials concluded that omega-3 fatty acid supplementation beneficially affects vascular endothelial function.232
Dietary Fiber
The term dietary fiber applies to a group of nondigestible elements that are not absorbed by the human body after eating. Insoluble fiber passes through the digestive tract unaltered, and soluble fiber can be fermented by intestinal microbes and broken down to short-chain fatty acids.233 Insoluble fiber is found in whole grains, wheat, bran, nuts and seeds. Soluble fiber is found in vegetables, fruits, legumes, oats, barley, and is the main type of fiber in fiber-based laxatives.
Numerous studies that observe cohort data over time have linked increased dietary fiber with a reduced risk of atherosclerosis, stroke, and peripheral vascular disease.219 In 2013, a review of 22 such studies spanning two decades and three continents found a significantly lower risk of atherosclerosis with greater intake of insoluble, cereal, fruit and vegetable fiber. The risk was lower with soluble fiber as well, but the association was not statistically significant.234
Randomized controlled studies involving fiber have focused mostly on cardiovascular disease risk factors. For example, a 2016 study randomized 60 post-menopausal women with elevated LDL cholesterol to receive brown rice extract supplements or placebo. At six months of treatment, those receiving the supplements had significantly lower levels of LDL cholesterol and TNF-α, a pro-inflammatory biochemical. Moreover, the rice bran extract also improved flow-mediated dilatation, a measure of vascular endothelial function.235
Polyphenols
Polyphenols, naturally occurring compounds found in tea, vegetables, fruits, and wine, are thought to counteract atherosclerosis by decreasing LDL oxidation, promoting NO levels, and inhibiting blood clot formation by reducing platelet clumping.219
In addition to being a source of monounsaturated fat, olive oil also contains polyphenols. A recent study examined the role of polyphenols in the protective effect of olive oil by providing participants with either olive oil enriched with its own polyphenols or regular olive oil. A small sample of individuals with mildly elevated blood pressure were given a single dose of either “boosted” or plain olive oil in a randomized blinded fashion. Those who received the “boosted” supplement saw an almost immediate improvement in endothelial function.236
Flavonols are another type of polyphenol found in fruits, vegetables, green tea, and cocoa. A major flavonol found in green tea and cocoa is catechin, which is thought to have a direct anti-inflammatory effect on vascular endothelial cells.237 In a small trial involving patients with heart failure, eating flavonol-rich chocolate led to an almost immediate improvement in vascular endothelial function when compared with plain chocolate, and sustained improvement after four weeks of daily consumption.238 Similarly, when 30 overweight men and women were given dark chocolate and a sugar-free cocoa beverage, vascular endothelial function improved compared with those given a low-flavonol chocolate bar and a cocoa-free beverage. The women in the study also saw an improvement in arterial stiffness with the administration of dark chocolate and cocoa.239
This effect may extend to black tea as well, which contains the polyphenols thearubigins and flavonoids. In a 2015 study, participants with high blood pressure drank a hot beverage containing a controlled amount of black tea-derived polyphenols. The researchers found that the polyphenol beverage dose-dependently improved blood pressure and arterial stiffness.240
Pine bark extract (Pycnogenol). Pycnogenol is obtained from the French maritime pine tree (Pinus pinaster). Between two-thirds and three-quarters of Pycnogenol is made up of catechins and their chemical cousins epicatechins.241,242 Pycnogenol benefits cardiovascular health through a variety of mechanisms. It has been demonstrated to inhibit inflammation and clotting, and improve endothelial function.243
In a randomized placebo-controlled trial, individuals with atherosclerosis received 200 mg Pycnogenol daily for eight weeks followed by placebo or vice versa. Treatment with Pycnogenol resulted in a significant reduction in oxidative stress and a 32% increase in a standardized measure of blood flow and vasodilation, a powerful indicator of endothelial function.244
Quercetin. Quercetin, a polyphenol found in apples, onions, cherries, and grapes, is known to possess anti-inflammatory and antioxidant properties, as well as a beneficial effect on diabetes and obesity.245 A controlled trial that tested quercetin supplements in 37 individuals with elevated blood pressure found improved measurements of inflammation linked to atherosclerosis as compared with placebo.246
Resveratrol. Resveratrol is another polyphenol found in grapes, berries, and peanuts. Historical studies have suggested it may have a positive treatment effect on atherosclerosis and high blood pressure.245 Resveratrol may inhibit the formation of foam cells and inhibit the uptake of ox-LDL.237 One animal study found that in mice fed a cholesterol-rich diet with and without resveratrol for 14 weeks, mice given resveratrol had atherosclerotic plaque regression and decreased plasma cholesterol levels.247
A study randomized 50 diabetic patients to receive either supplemental resveratrol or placebo for 12 weeks, then measured a number of physiologic and metabolic parameters and compared them to parameters determined at baseline. The study concluded that resveratrol not only improved blood pressure and body weight, but also reduced arterial stiffness, a common surrogate for atherosclerosis.248
Hesperidin. Hesperidin is a polyphenol that occurs in citrus fruits, especially their peels.249,250 Digestion of hesperidin produces a compound called hesperetin, along with other metabolites. These compounds are powerful free radical scavengers and have demonstrated anti-inflammatory, insulin-sensitizing, and lipid-lowering activity.251,252
In a randomized, placebo-controlled, crossover trial, 24 adults with metabolic syndrome were treated with 500 mg of hesperidin per day or placebo for three weeks. Hesperidin treatment improved endothelial function, suggesting this may be one important mechanism behind its cardiovascular benefits. Hesperidin supplementation also led to a 32% reduction in CRP, as well as significant decreases in levels of total cholesterol, apolipoprotein B, and markers of vascular inflammation, relative to placebo.253
Hydroxytyrosol. Hydroxytyrosol, the main phenol found in olive oil, is a potent antioxidant and anti-inflammatory agent that may inhibit LDL oxidation, platelet aggregation, and atherosclerosis progression.237,254 In one randomized crossover trial involving 200 healthy males, participants received 25 mL of three olive oils (one with 2.7 mg/kg of phenolic compounds, one with 164 mg/kg of phenolic compounds, and one with 366 mg/kg of phenolic compounds) for three weeks, followed by a two week washout period between treatments. HDL cholesterol levels increased and triglyceride levels decreased in all groups, and oxidative stress markers decreased linearly depending on phenolic content of the oil. Researchers concluded that the benefits of olive oil were greater than its monounsaturated fatty acid content, and that phenolic compounds in the oil may benefit plasma lipid levels and help prevent oxidative damage.255
In another randomized, double-blind, crossover study involving 13 early-stage hypertensive patients, subjects received 30 mg of functional olive oil enriched with its own polyphenols or standard virgin olive oil. Markers of endothelial function were followed for five hours after oil consumption. The enriched oil demonstrated greater benefit than the standard oil.236
Green Coffee Bean Extract
Green coffee beans are higher in chlorogenic acids compared with roasted coffee beans, which are typically used to make coffee beverages. A meta-analysis of data from 14 randomized controlled trials with a combined total of 821 participants found green coffee bean extract, at doses of 180–376 mg daily, improved cardiometabolic health by reducing triglyceride levels and systolic and diastolic blood pressures, and increasing high-density lipoprotein (HDL)-cholesterol levels.452 Another meta-analysis that included 15 randomized controlled trials with a total of 637 participants found green coffee extract also lowered total cholesterol and fasting blood glucose levels.453 Other meta-analyses have also reported green coffee extract’s positive effects on lipid levels, glucose metabolism, and blood pressure.454-456 A placebo-controlled crossover trial in 21 healthy middle-aged volunteers found a single dose of 302 mg of decaffeinated green coffee extract (but not higher doses) improved blood vessel function up to 24 hours post-dose.457 Another placebo-controlled trial in 16 healthy men found blood vessel function and a measure of arterial stiffness improved after two weeks of supplementing with a green coffee bean beverage.458
Phytosterols
Phytosterols, plant compounds similar in nature to cholesterol, help support healthy LDL levels by competing with cholesterol for uptake into cells. As previously highlighted, cholesterol plays a role in the development of cardiovascular disease and atherosclerosis.237 Phytosterols can be found in rice bran, wheat germ, corn oils, soybeans, and peanuts.
In a randomized, double-blind, placebo-controlled trial, 232 men and women with elevated cholesterol levels consumed 20 grams per day of a low-fat spread with or without plant sterols (3 grams per day) for 12 weeks. Serum LDL levels were reduced with phytosterol supplementation.256 In a meta-analysis of 20 randomized controlled trials involving over 1,300 subjects, there was a clear association between phytosterol intake and reduced serum LDL cholesterol levels.257 In an older cross-sectional study of over 22,000 men and women aged 39‒79, researchers concluded that a high intake of plant sterols was associated with lower total and LDL cholesterol levels.258
Beta-sitosterol is a plant sterol associated with healthy cholesterol levels and optimal cardiovascular health. It is also believed to combat obesity-related inflammation, and may help treat metabolic diseases.259 Research in hypertensive rats with renal damage suggests treatment with beta-sitosterol (at a dose between 1.3‒2.3 mg/kg) for two weeks decreased atherosclerotic markers, including total cholesterol, LDL, and triglyceride levels.260
Vitamins
B vitamins. The family of B vitamins includes eight compounds: thiamine (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5), pyridoxine (B6), biotin (B7), folate (B9) and cobalamin (B12). They play a role in energy production and cellular health, and are found in fish, leafy greens, and liver.261 Data suggest the B vitamin family plays a role in maintaining optimal cardiovascular health. In a randomized controlled study involving over 300 people, subjects with the highest intake of a variety of micronutrients, including vitamin B6, folate, and antioxidants, had the lowest risk of stroke and cerebral atherosclerosis.262
In another trial involving 81 people with mild-to-moderately high blood pressure who were not on blood pressure medication, a combination of L-arginine (2.4 grams) and vitamin B6 (3 mg), folic acid (0.4 mg), and vitamin B12 (2 mcg) improved vascular function (including blood pressure, endothelial health, and homocysteine levels) compared with placebo.263
Niacin (vitamin B3), which is involved in energy production and cellular communications and function, is found in poultry, meat, and fish.264 Research has long suggested that niacin plays a role in maintaining cardiovascular health, including decreasing coronary artery disease and strokes.265,266 Animal research suggests niacin inhibits atherosclerosis and decreases levels of inflammatory cytokines.267 A randomized placebo-controlled study of over 300 patients with coronary heart disease (with LDL cholesterol levels less than 100 mg/dL and HDL cholesterol levels less than 50 mg/dL) on statins found that 2,000 mg per day of niacin was more effective than 10 mg/day of ezetimibe at reducing carotid thickness after 14 months.268
Vitamins C and E. Vitamin C, a potent antioxidant and water-soluble vitamin that helps synthesize collagen, metabolize protein, and heal wounds, is found naturally in broccoli and oranges.269 Vitamin E, a fat-soluble vitamin found naturally in nuts, seeds, and vegetable oils, is a potent antioxidant that plays a role in immune function and cell signaling.270 Vitamin E is actually a family of eight different compounds, including four tocopherols and four tocotrienols. Research suggests it may be cardioprotective and exert control over the atherosclerotic process via microRNA regulation.271
Older cellular and animal models demonstrate that vitamin C improves endothelial function.237 A population-based prospective study involving over 20,000 people suggests vitamin C concentrations are associated with a decreased risk of stroke.272 In an older trial, 520 men and post-menopausal women (including smokers and non-smokers) took 136 IU vitamin E and 250 mg of slow-release vitamin C. At the three year follow-up, supplementation slowed the progression of atherosclerosis in men, and at the six year follow-up, a similar result was seen in both genders (but more significantly in males).273
While clinical trials involving vitamin E’s cardioprotective abilities have been mixed, some scientists believe this is the result of type of tocopherol compounds studied, particularly the lack of gamma-tocopherol, which has potent antioxidant and anti-inflammatory effects. Further research, particularly in the form of randomized clinical trials, is warranted for both vitamins.274
Vitamin K. Vitamin K, a fat-soluble family of vitamin compounds, plays a role in blood clotting and bone metabolism. Vitamin K1 is naturally found in leafy green vegetables, while K2 is mainly found in fermented foods like cheeses and natto (fermented soybeans).119,377 Importantly, adequate vitamin K intake is critical for helping maintain healthy calcium balance in the arteries and bones. In fact, older anticoagulant drugs, such as warfarin, block the activity of vitamin K and are associated with increased vascular calcification.120 Conversely, vitamin K supplementation (especially K2 supplementation) slows the progression of coronary artery calcification in people with pre-existing coronary calcification and helps improve vascular stiffness.121-123
In a study of 42 people with chronic kidney disease, participants took either 10 mcg cholecalciferol (vitamin D3) or a combination of 90 mcg menaquinone (vitamin K2) and 10 mcg cholecalciferol for 270 days. The group taking vitamin K plus vitamin D showed lower carotid arterial thickness, suggesting the combination slowed the progression of atherosclerosis.275 In a randomized controlled trial published in 2015, supplementation with 180 mcg menaquinone-7 (MK-7, a form of vitamin K2) was compared with placebo in 244 healthy postmenopausal women. After three years the women taking MK-7 exhibited decreased arterial stiffness compared with those taking placebo.122 Similar results were obtained in a smaller, single-arm trial among renal transplant recipients taking 360 mcg MK-7 daily for eight weeks.123
A 2020 meta-analysis of three cohort studies analyzed the association of vitamin K1 concentrations with cardiovascular disease and mortality from any cause. The results from 3,891 participants indicated that while there was no significant difference in cardiovascular disease risk with K1 levels, the risk of all-cause mortality was 19% higher in those with the lowest circulating K1 levels.378
Coenzyme Q10
Coenzyme Q10 (CoQ10) is a naturally occurring antioxidant that plays an important role in cellular energy metabolism. Statin therapy significantly lowers blood CoQ10 levels,276 and for this reason many health care providers recommend CoQ10 supplementation for those taking statins.
CoQ10 deficiency is associated with an increased risk of cardiovascular disease. Several publications suggest that CoQ10 has beneficial effects on CRP and levels of pro-inflammatory biochemicals.277 After one year of supplementing with CoQ10 and aged garlic extract, a small trial of healthy, nonsmoking firefighters found an improvement in measures of arterial stiffness and endothelial function compared with placebo.278 In this same group, calcium artery scores were used to estimate risk of atherosclerosis. Before treatment, the average calcium score was in the moderate range. Supplementation slowed the rate of increase of the average calcium score by a statistically significant amount, suggesting the combination of CoQ10 and aged garlic extract may slow the progression of atherosclerosis before it becomes clinically evident.279
A review of five well-controlled studies established that CoQ10 supplementation improved vascular endothelial function in patients with known atherosclerosis or significant risk factors for atherosclerosis, like high cholesterol and diabetes.280 Macrophages isolated from the blood of healthy volunteers that were given 100 mg CoQ10 for one week proved resistant to foam cell formation compared with those from people who received placebo through increased cholesterol removal from cells.281 A recent cellular study found that CoQ10 may play a role in reducing atherosclerotic plaques by inhibiting a platelet signaling pathway.282
Magnesium
Magnesium plays several important roles in cardiovascular health.283 Accordingly, magnesium deficiency can contribute to several problems with cardiovascular physiology.283 Clinical studies have shown that magnesium supplementation can favorably modulate parameters related to cardiovascular health, including blood pressure,284 endothelial function,285 arterial stiffness and calcification,286,287 and hs-CRP levels,288 among others. Observational evidence suggests greater magnesium intake is associated with lower mortality among people at high risk of cardiovascular disease.289
Propionyl-L-carnitine
Propionyl-L-carnitine has received attention for its ability to decrease the severity of atherosclerotic lesions in animals.290 Propionyl-L-carnitine is a chemical made in the body that rapidly passes into cells across the mitochondrial membrane to supply free carnitine, a much-needed factor for energy production.291 Carnitines are essential for mitochondrial fatty acid transport and energy production, which is important because endothelial cells and heart muscle cells mostly burn fatty acids as their source of energy.292
Animal studies suggest propionyl-L-carnitine may help prevent or decrease the severity of vascular disease. In rabbits fed a high-cholesterol diet, which normally induces endothelial dysfunction and subsequent atherosclerosis, supplementation with propionyl-L-carnitine resulted in reduced plaque thickness, markedly lowered triglyceride levels, and reduced proliferation of foam cells.290 In a rat study, propionyl-L-carnitine accelerated wound healing, reduced oxidative stress, and improved vascular function.293 In human studies, propionyl-L-carnitine produced significant improvement in maximum walking distance in those with claudication (pain while walking due to atherosclerosis in the legs), with no major side effects.294
Carnosine
Carnosine is an antioxidant that naturally occurs in meat sources, and therefore is often lacking from a vegetarian diet. Carnosine is a dipeptide (two amino acids linked together) composed of the amino acids L-histidine and beta-alanine. In the body, carnosine can counteract oxidative stress and improve muscle contractions.295
In the laboratory, when added to cultures of human macrophages, carnosine inhibited the formation of foam cells.296 Animal research suggests the antioxidant, anti-inflammatory, and chelating properties of carnosine make it potentially therapeutic for cardiovascular and metabolic disorders.297 A pilot study in overweight individuals demonstrated improved insulin resistance after three months of carnosine supplementation, leading some experts to hypothesize that carnosine may prove to be useful in controlling atherosclerosis risk factors, particular in diabetes.237,298
Lipoic Acid
Lipoic acid, a naturally occurring antioxidant, serves as a coenzyme in energy metabolism of fats, carbohydrates, and proteins. It can regenerate thioredoxin (an antioxidant protein), vitamin C, and glutathione, which in turn can recycle vitamin E. Lipoic acid also helps manage proper serum glucose levels in diabetic patients.299 Research suggests that lipoic acid decreases oxidative stress, which may promote optimal cardiovascular health.300
In a rabbit model of atherosclerosis, rabbits were fed a high cholesterol diet with and without lipoic acid supplements for three months. Those that received the supplements demonstrated a reduction in atherosclerotic plaque formation as determined by MRI of their abdominal aortas.301 In a randomized placebo-controlled clinical trial in 58 patients with metabolic syndrome, one month of lipoic acid supplementation improved vascular endothelial function and reduced levels of pro-inflammatory biochemicals.302
Glucosamine
Known best as a supplement for combating osteoarthritis and joint pain, glucosamine may have benefits above and beyond these indications. In a recent randomized controlled trial, 3,000 mg glucosamine for four weeks improved vascular endothelial function.303 In another questionnaire-based study of nearly 78,000 people from Washington state found that regular glucosamine use was associated with a non-significant 12% reduced risk of death from cardiovascular disease, as well as significantly associated with a reduced risk of death from cancer, respiratory illness, and all other causes.304
Findings from the United Kingdom’s health resource databank, UK Biobank, published in early 2019 suggested people taking glucosamine supplements for arthritis have a lower risk of death from cardiovascular disease, atherosclerosis, and heart attack and stroke, even after statistically adjusting the data to remove influence from age, gender, BMI, race, lifestyle factors, dietary intake, drug use, and other supplement use.305
Selenium
Selenium, an antioxidant and trace mineral naturally found in seafood and organ meats, is essential for DNA synthesis, reproduction, and protection from oxidative damage.306 Animal research suggests selenium supplementation may be cardioprotective, and that it prevents atherosclerosis by inhibiting oxidative stress, suppressing endothelial dysfunction, and modulating inflammation.307
In a controlled study involving mice, animals fed a diet fortified with selenium (0.3 mg/kg) had reduced plaque lesion formation.308 A cellular model of atherosclerosis demonstrated that selenium and vitamin D attenuated monocyte adhesion to endothelial cells.309 This suggests these nutrients may play a role in modulating the atherosclerotic process. However, further study is necessary to confirm the role selenium plays in preventing atherosclerosis.
L-Arginine
L-arginine, typically found in meat, fish, and soy, is an amino acid that has attracted attention for its ability to improve endothelial function and dilate blood vessels. L-arginine serves as the precursor of NO in the endothelium.310,311 Cell line and animal studies suggest L-arginine decreases inflammation and reduces vascular dysfunction.312-314 In a human study looking at the effects of oral L-arginine in patients with stable coronary artery disease, 10 grams L-arginine daily improved brachial artery dilation, a measure of endothelial function, and reduced LDL oxidation.315
Arginine Silicate
Arginine silicate, a specialized form of arginine stabilized with inositol, has been shown to boost NO levels and may represent a novel form of arginine with potential benefits in cardiovascular health.316 Interestingly, arginine silicate has also been shown to improve some aspects of cognitive function in a clinical trial in healthy young men. These results were postulated to be related to improved blood flow.317 In a rat model of kidney and cardiovascular disease, arginine silicate improved some measures of vascular function and manifestations of kidney damage.318
Aronia melanocarpa
Aronia melanocarpa, also called black chokeberry, is a member of the rose family. It produces small berries rich in polyphenols. In a clinical trial, 66 healthy male adults consumed an aronia extract containing 40% total polyphenols daily for 12 weeks. The aronia extract led to a significant improvement in flow-mediated dilation, a measure of vascular function. Aronia extract supplementation also led to potentially beneficial modifications of the gut microbiota. The authors of the study concluded that “…daily consumption of aronia berry polyphenols…has the potential to maintain cardiovascular health in healthy individuals at low risk of cardiovascular disease.”319 In a pre-clinical study, aronia extract, at relatively low concentrations, increased NO production by bovine endothelial cells.320
Red Yeast Rice
Red yeast rice is a fermented type of rice that contains naturally occurring compounds called monacolins that reduce LDL cholesterol with the same mechanism as statins. In those who cannot tolerate the side effects of statins, red yeast rice can be considered as an acceptable substitute.321 One well-controlled clinical trial using red yeast rice extract in individuals with prior heart attack and not taking any cholesterol-lowering medication showed that the supplement cut the incidence of heart attack and cardiovascular death by nearly one-half.322
Notably, there is evidence that red yeast rice supplements can be appropriate for adults of all ages, including the elderly.219 Also, the LDL-lowering effects can be appropriate for younger individuals, based on a controlled trial that showed a supplement containing red yeast rice to be safe and effective in LDL-lowering in people as young as 18 years old.323
In a recent animal study, red yeast rice decreased plaque formation and cholesterol levels in mice with atherosclerosis on a high-fat diet. The red yeast rice structurally changed the intestinal microflora, improved intestinal barrier function, and mediated inflammatory signaling pathways. The authors concluded that red yeast rice could alter gut microflora, which was protective against atherosclerosis.324
Garlic
Allicin is a naturally occurring substance that is released when fresh garlic is crushed. The chemical reaction creates hydrogen sulfide, which may have properties that counteract atherosclerosis.237 Aged garlic extract also contains similar sulfur-based compounds that have antioxidant effects protective against vascular endothelial damage.325
Garlic powder supplements were found to decrease atherosclerosis plaque progression in a placebo-controlled trial of 152 people with advanced carotid and/or femoral plaque as determined by ultrasound.326 In a thorough review of randomized controlled trials and meta-analyses, garlic supplementation was found to help reduce blood pressure and cholesterol levels. Aged garlic extract was especially effective at improving CRP and coronary artery calcification.61
Curcumin
Curcumin is an active ingredient in turmeric, a spice commonly used in curry. Because of its antioxidant properties, it has been studied in human atherosclerosis trials. A study of 32 healthy but sedentary post-menopausal women compared curcumin supplementation to exercise, which is known to improve vascular endothelial function. After eight weeks, the supplement group displayed an improvement in endothelial function that was as good as a supervised moderate aerobic exercise program. A control group which received neither curcumin supplements nor an exercise program showed no change in endothelial function.327 Recent animal research suggests a novel, soluble form of curcumin promotes plaque stability and reduces the development of atherosclerosis.328
In a trial of 240 men and women with type 2 diabetes and a low incidence (6%) of established atherosclerosis that received curcumin supplementation for six months, researchers found an improvement in endothelial function in the group receiving supplements compared with the placebo group. Interestingly, curcumin supplementation led to a significant decrease in leptin levels in the blood as well.329 As noted elsewhere, excess levels of leptin resulting from leptin resistance causes endothelial dysfunction, inflammatory stress, and promotes thrombosis.328
Carotenoids
Lycopene. Lycopene, an antioxidant carotenoid found in tomatoes and other fruits and vegetables, has several properties that may protect against atherosclerosis. These mechanisms include the ability to reduce inflammation, decrease cholesterol production, and inhibit smooth muscle proliferation.330 In a controlled trial involving patients with stable cardiovascular disease, adding lycopene to existing statin therapy led to a significant improvement in endothelial function. No effect on endothelial function was observed in age-matched healthy controls.331
A meta-analysis of six studies concluded that consuming tomatoes, which is a rich source of lycopene and other carotenoids, reduced total and LDL cholesterol levels and triglyceride levels while raising HDL levels.388 In addition, lycopene itself has been shown to improve systolic blood pressure and decrease the risk of stroke and coronary heart disease.389
Heart rate variability is an indicator of cardiac autonomic health. In a cross-sectional analysis of a general US adult population, blood levels of several carotenoids were associated with higher heart rate variability, a beneficial marker for heart health. The carotenoids included lycopene, alpha [α]-carotene, and all-trans-beta-carotene, and the association remained significant even after adjusting for several factors related to heart health such as age, weight, and smoking habits. The authors of the study suggested that daily intake of fruits and vegetables to increase blood carotenoid status may help prevent autonomic dysfunction.390
Lycopene’s capacity to reduce inflammation was highlighted in a 2016 controlled trial in 40 healthy volunteers. In this study, a single meal of tomatoes or tomato sauce reduced blood levels of inflammatory biochemicals, and this effect was enhanced when refined olive oil was added to the meal.12
Carotenes. Carotenes are plant pigments required by many plants and present in many vegetables, including carrots, pumpkin, and green leafy vegetables.391 It is widely accepted that high intake of fruits and vegetables is protective against heart disease. In a Japanese study in several hundred participants, serum carotenoid levels, including lycopene, beta-carotene and lutein, were associated with lower visceral fat area in women. Visceral fat is a powerful risk factor for cardiovascular disease.392 Additionally, as mentioned above, blood levels of α-carotene and all-trans-beta-carotene were associated with higher heart rate variability.390
Xanthophylls. Xanthophylls are a class of carotenoids that includes lutein and zeaxanthin, which are mostly known for their impact on eye health. However, their anti-inflammatory effects may have a role in cardiometabolic health as well.393 Lutein and zeaxanthin levels were inversely associated with levels of the inflammatory cytokine interleukin-6 (IL-6) in coronary artery disease patients and showed strong anti-inflammatory effects in peripheral blood mononuclear cells.394 In a meta-analysis of 71 studies that included nearly 390,000 participants, higher dietary intake and higher blood concentration of lutein was associated with better cardiometabolic health, including a lower risk of coronary heart disease and stroke.395 Lutein has many anti-atherosclerotic effects, including improving endothelial function and arterial thickness and reducing blood pressure. Lutein may also improve lipid profiles.393 In an animal model of myocardial infarction, lutein exhibited cardioprotective benefits and decreased inflammation.396
Saffron
Known best as a cooking spice and natural coloring agent, saffron has also been used as a medicinal plant for its pain-relieving and anticancer properties. Because of some promising animal studies showing an improvement in atherosclerosis plaque formation, there is interest in studying saffron as a treatment for atherosclerosis.333 A controlled trial involving 105 participants with the constellation of heart disease risk factors called metabolic syndrome found that saffron supplementation reduced amounts of antibodies to heat shock proteins.334 These antibodies are thought to have a role in accelerating the atherosclerosis disease process,335 and reducing them may therefore have a protective effect. In a randomized double-blind clinical trial, 63 people with atherosclerosis received either 100 mg saffron or placebo daily for six weeks. Those in the treatment group showed altered expression of the microRNAs that regulate gene expression of biomarkers of cardiovascular disease.336
Capsaicin
The ingredient in hot peppers that provides heat to the spice has also been shown in animal models to have beneficial effects on vascular endothelial function and atherosclerosis progression.337 Interestingly, according to a small but well-controlled study, applying a capsaicin patch on individuals with atherosclerosis prior to an exercise stress test enhanced blood NO levels.338 As mentioned elsewhere, NO is a naturally occurring biochemical that lowers blood pressure and increases blood flow. In individuals with low levels of the protective HDL cholesterol, three months of capsaicin supplements raised HDL levels and decreased triglyceride and CRP levels compared with placebo.339 In a randomized animal model study, guinea pigs fed a high-fat diet that received 2.5‒10 mg/kg capsaicin demonstrated reduced oxidative stress and improved endothelial function. All doses of capsaicin decreased total cholesterol and triglyceride levels and increased HDL cholesterol levels.340
Centella asiatica
Centella asiatica (commonly known as Gotu Kola) is a perennial herbaceous plant used in traditional Ayurvedic and Chinese medicine for thousands of years.341 The most important bioactive components in C. asiatica are triterpenes, which may have plaque-stabilizing abilities.342 Centella’s benefit to the vascular endothelium appears to be related, at least in part, to anti-inflammatory activity, modulation of collagen formation, and oxidative stress reduction.343
In two randomized controlled trials in patients with atherosclerosis, supplementation with 60 mg of a triterpenoid extract of C. asiatica three times daily for 12 months stabilized atherosclerotic plaques in femoral and carotid arteries.342,344 In another study that followed over 300 people with asymptomatic atherosclerosis for four years, the use of a C. asiatica and Pycnogenol extract (100 mg of each) was better than diet and exercise or Pycnogenol supplementation (100 mg) alone at reducing plaque progression and oxidative stress.345 The authors concluded that the results are promising and warrant a larger study.
Ginkgo Biloba
Ginkgo biloba is an extract from leaves of the tree of the same name (also known as the maidenhair tree). This extract has traditionally been used for thousands of years to promote cardiovascular health, relax the lungs, and as a circulatory system tonic.346 Several in vitro studies have shown that ginkgo may favorably alter endothelial function and reduce levels of ox-LDL.347-349
In a study involving eight patients who had recently undergone coronary artery bypass surgery, supplementation with ginkgo biloba extract, at 120 mg twice daily, was shown to reduce atherosclerotic plaque formation. Furthermore, ginkgo increased levels of endogenous antioxidant enzymes and reduced levels of ox-LDL.350 Studies of ginkgo biloba supplementation in humans have also demonstrated an improvement in claudication (pain while walking due to atherosclerosis in the legs).351 For this reason, ginkgo biloba is used commonly in Europe for symptoms of peripheral arterial disease.
Policosanol
Policosanol is an extract from the waxy coating of sugar cane. Research in rats with high cholesterol levels indicates that policosanol increased fecal cholesterol content and inhibited cholesterol biosynthesis and LDL cholesterol uptake.352 A randomized controlled study of hypertensive rats found that after eight weeks, policosanol (at doses of 20, 100, and 200 mg/kg) reduced blood pressure levels in a dose-dependent manner. Markers of hepatic inflammation and triglyceride levels were decreased and HDL cholesterol levels were elevated in the treatment groups.353
An older prospective, randomized, double-blind, placebo-controlled trial involved nearly 590 people with high cholesterol and blood pressure levels taking either 5 mg policosanol or placebo daily for 12 months. After six months, the policosanol dosage was doubled in those with cholesterol levels greater than 6.1 mmol/L. Policosanol decreased blood pressure, cholesterol, and increased HDL cholesterol levels compared with placebo.354 Further research is warranted to determine how policosanol impacts cardiovascular health.
Guggul
Guggul is a plant extract traditionally used to ameliorate arthritis, urinary tract disorders, and skin conditions.355 An animal study concluded that 3.5 mg/kg of guggul, alone and in combination with 3.7 mg/kg of atorvastatin, lowered cholesterol, LDL, VLDL, and triglyceride levels compared with control rabbits fed a high-fat diet.356 In another study involving mice fed a high-fat diet for 16 weeks, a combination of Curcuma longa, silymarin, guggul, chlorogenic acid, and inulin altered inflammatory activity and lipid metabolism, which may play a role in modulating atherosclerotic development.357 Older human research suggests guggul may support healthy cholesterol levels,358 but more clinical research is warranted.
Hawthorn
Hawthorn, a flower shrub of the rose family, has traditionally been used to treat heart, digestive, and kidney problems, and to combat anxiety.359 A mouse study found that 50 mg/kg hawthorn extract daily for 16 weeks decreased inflammatory markers as well as triglyceride, total cholesterol, and LDL cholesterol levels and increased HDL cholesterol levels.360 Another animal model study found that hawthorn attenuated atherosclerotic lesion area, inhibited foam cell formation, and altered the expression of genes involved with antioxidant activities. This is suggestive of hawthorn’s potential therapeutic use in preventing atherosclerosis.361
Potassium
Potassium, found naturally in fruits, vegetables, legumes, and potatoes, is an essential nutrient that is vital to cellular functioning.362 A recent animal study indicated that reduced dietary potassium intake was associated with arterial stiffness and atherosclerotic vascular calcification. The authors postulated that reduced potassium concentrations increased intracellular calcium levels.363
Increasing potassium intake and reducing sodium intake has been associated with reduced cardiovascular risk. As noted in the section titled “Adopt a Healthy Diet,” data from six prospective cohort studies showed that each daily increment of 1,000 mg potassium excretion was associated with an 18% decreased cardiovascular risk.420 In addition, a large open-label trial that included over 20,000 participants in rural China, most of whom were over age 60 and had a history of stroke and hypertension, showed that substituting regular sodium salt with a salt containing 25% potassium chloride significantly reduced the rates of several cardiovascular events.421
2022
- Oct: Added section on coffee consumption and cardiovascular disease to Atherosclerosis Prevention
- Oct: Added section on green coffee bean extract to Nutrients
- Mar: Updated section on adopting a healthy diet in Atherosclerosis Prevention
- Mar: Updated section on potassium in Nutrients
2021
- Nov: Added section on TMAO and cardiovascular disease to Atherosclerosis Risk Factors
- May: Added section on carotenoids to Nutrients
- May: Updated section on physical activity in Atherosclerosis Prevention
2019
- Dec: Comprehensive update & review
Disclaimer and Safety Information
This information (and any accompanying material) is not intended to replace the attention or advice of a physician or other qualified health care professional. Anyone who wishes to embark on any dietary, drug, exercise, or other lifestyle change intended to prevent or treat a specific disease or condition should first consult with and seek clearance from a physician or other qualified health care professional. Pregnant women in particular should seek the advice of a physician before using any protocol listed on this website. The protocols described on this website are for adults only, unless otherwise specified. Product labels may contain important safety information and the most recent product information provided by the product manufacturers should be carefully reviewed prior to use to verify the dose, administration, and contraindications. National, state, and local laws may vary regarding the use and application of many of the therapies discussed. The reader assumes the risk of any injuries. The authors and publishers, their affiliates and assigns are not liable for any injury and/or damage to persons arising from this protocol and expressly disclaim responsibility for any adverse effects resulting from the use of the information contained herein.
The protocols raise many issues that are subject to change as new data emerge. None of our suggested protocol regimens can guarantee health benefits. Life Extension has not performed independent verification of the data contained in the referenced materials, and expressly disclaims responsibility for any error in the literature.
- Clinic M. Arteriosclerosis / atherosclerosis. https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569. Published 2018. Accessed October 21, 2019.
- Association AH. Atherosclerosis. https://www.heart.org/en/health-topics/cholesterol/about-cholesterol/atherosclerosis. Published 2017. Accessed October 21, 2019.
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146-e603.
- Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56-e528.
- Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Journal of the American College of Cardiology. 2012;60(24):e44-e164.
- Alpert JS. A few unpleasant facts about atherosclerotic arterial disease in the United States and the world. Am J Med. 2012;125(9):839-840.
- Bian F, Yang X, Zhou F, et al. C-reactive protein promotes atherosclerosis by increasing LDL transcytosis across endothelial cells. Br J Pharmacol. 2014;171(10):2671-2684.
- Kim JM, Park KY, Shin DW, Park MS, Kwon OS. Relation of serum homocysteine levels to cerebral artery calcification and atherosclerosis. Atherosclerosis. 2016;254:200-204.
- Eltoft A, Arntzen KA, Hansen JB, Wilsgaard T, Mathiesen EB, Johnsen SH. C-reactive protein in atherosclerosis - A risk marker but not a causal factor? A 13-year population-based longitudinal study: The Tromso study. Atherosclerosis. 2017;263:293-300.
- Quaglia LA, Freitas W, Soares AA, et al. C-reactive protein is independently associated with coronary atherosclerosis burden among octogenarians. Aging clinical and experimental research. 2014;26(1):19-23.
- Bergheanu SC, Bodde MC, Jukema JW. Pathophysiology and treatment of atherosclerosis : Current view and future perspective on lipoprotein modification treatment. Neth Heart J. 2017;25(4):231-242.
- Valderas-Martinez P, Chiva-Blanch G, Casas R, et al. Tomato Sauce Enriched with Olive Oil Exerts Greater Effects on Cardiovascular Disease Risk Factors than Raw Tomato and Tomato Sauce: A Randomized Trial. Nutrients. 2016;8(3):170.
- Prasad K. Pathophysiology and Medical Treatment of Carotid Artery Stenosis. The International journal of angiology : official publication of the International College of Angiology, Inc. 2015;24(3):158-172.
- Bennett MR, Sinha S, Owens GK. Vascular Smooth Muscle Cells in Atherosclerosis. Circ Res. 2016;118(4):692-702.
- Tabas I, Bornfeldt KE. Macrophage Phenotype and Function in Different Stages of Atherosclerosis. Circ Res. 2016;118(4):653-667.
- Gimbrone MA, Jr., Garcia-Cardena G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ Res. 2016;118(4):620-636.
- Sakakura K, Nakano M, Otsuka F, Ladich E, Kolodgie FD, Virmani R. Pathophysiology of atherosclerosis plaque progression. Heart Lung Circ. 2013;22(6):399-411.
- Napoli C, D'Armiento FP, Mancini FP, et al. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J Clin Invest. 1997;100(11):2680-2690.
- Hong YM. Atherosclerotic cardiovascular disease beginning in childhood. Korean circulation journal. 2010;40(1):1-9.
- Insull W, Jr. The pathology of atherosclerosis: plaque development and plaque responses to medical treatment. Am J Med. 2009;122(1 Suppl):S3-s14.
- Yahagi K, Kolodgie FD, Lutter C, et al. Pathology of Human Coronary and Carotid Artery Atherosclerosis and Vascular Calcification in Diabetes Mellitus. Arteriosclerosis, thrombosis, and vascular biology. 2017;37(2):191-204.
- Rennenberg RJMW, Kessels AGH, Schurgers LJ, van Engelshoven JMA, de Leeuw PW, Kroon AA. Vascular calcifications as a marker of increased cardiovascular risk: a meta-analysis. Vascular health and risk management. 2009;5(1):185-197.
- Kalampogias A, Siasos G, Oikonomou E, et al. Basic Mechanisms in Atherosclerosis: The Role of Calcium. Medicinal chemistry (Shariqah (United Arab Emirates)). 2016;12(2):103-113.
- Neves PO, Andrade J, Moncao H. Coronary artery calcium score: current status. Radiol Bras. 2017;50(3):182-189.
- Orimoloye OA, Banga S, Dardari ZA, et al. Coronary artery calcium as a predictor of coronary heart disease, cardiovascular disease, and all-cause mortality in Asian-Americans: The Coronary Artery Calcium Consortium. Coronary artery disease. 2019.
- Association AH. Aspirin and Heart Disease. https://www.heart.org/en/health-topics/heart-attack/treatment-of-a-heart-attack/aspirin-and-heart-disease. Published 2019. Accessed October 22, 2019.
- National Heart L, and Blood Institiute. Atherosclerosis. https://www.nhlbi.nih.gov/health-topics/atherosclerosis. Published 2018. Accessed October 21, 2019.
- Husain K, Hernandez W, Ansari RA, Ferder L. Inflammation, oxidative stress and renin angiotensin system in atherosclerosis. World J Biol Chem. 2015;6(3):209-217.
- Lovren F, Teoh H, Verma S. Obesity and atherosclerosis: mechanistic insights. The Canadian journal of cardiology. 2015;31(2):177-183.
- Shah A, Mehta N, Reilly MP. Adipose inflammation, insulin resistance, and cardiovascular disease. JPEN Journal of parenteral and enteral nutrition. 2008;32(6):638-644.
- Ortega SP, Chouchani ET, Boudina S. Stress turns on the heat: Regulation of mitochondrial biogenesis and UCP1 by ROS in adipocytes. Adipocyte. 2017;6(1):56-61.
- Paoletti R, Bolego C, Poli A, Cignarella A. Metabolic syndrome, inflammation and atherosclerosis. Vasc Health Risk Manag. 2006;2(2):145-152.
- Wu SH, Liu Z, Ho SC. Metabolic syndrome and all-cause mortality: a meta-analysis of prospective cohort studies. European journal of epidemiology. 2010;25(6):375-384.
- Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. Journal of the American College of Cardiology. 2010;56(14):1113-1132.
- KEYS A. Human Atherosclerosis and the Diet. Circulation. 1952;5(1):115-118.
- Saita E, Kondo K, Momiyama Y. Anti-Inflammatory Diet for Atherosclerosis and Coronary Artery Disease: Antioxidant Foods. Clinical Medicine Insights Cardiology. 2015;8(Suppl 3):61-65.
- Association AH. The American Heart Association Diet and Lifestyle Recommendations. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/aha-diet-and-lifestyle-recommendations. Published 2018. Accessed October 21, 2019.
- Al-Mamari* A. Atherosclerosis and Physical Activity. Oman medical journal. 2009;24.
- Paffenbarger RS, Jr., Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. The New England journal of medicine. 1986;314(10):605-613.
- Schroeder TE, Hawkins SA, Hyslop D, Vallejo AF, Jensky NE, Wiswell RA. Longitudinal change in coronary heart disease risk factors in older runners. Age Ageing. 2007;36(1):57-62.
- Oldridge N, Gottlieb M, Guyatt G, Jones N, Streiner D, Feeny D. Predictors of health-related quality of life with cardiac rehabilitation after acute myocardial infarction. J Cardiopulm Rehabil. 1998;18(2):95-103.
- Center UoRM. What You Can Do to Prevent Atherosclerosis. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=1&contentid=1583. Published 2019. AccessedOctober 21, 2019.
- Tell GS, Polak JF, Ward BJ, Kittner SJ, Savage PJ, Robbins J. Relation of smoking with carotid artery wall thickness and stenosis in older adults. The Cardiovascular Health Study. The Cardiovascular Health Study (CHS) Collaborative Research Group. Circulation. 1994;90(6):2905-2908.
- Head T, Daunert S, Goldschmidt-Clermont PJ. The Aging Risk and Atherosclerosis: A Fresh Look at Arterial Homeostasis. Frontiers in genetics. 2017;8:216-216.
- Pandey AK, Blaha MJ, Sharma K, et al. Family history of coronary heart disease and the incidence and progression of coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2014;232(2):369-376.
- U.S. National Library of Medicine. Cholesterol. https://medlineplus.gov/cholesterol.html. Accessed November 12, 2019.
- Leiva E, Wehinger S, Guzman L, Orrego R. Role of Oxidized LDL in Atherosclerosis. In: Kumar SA, ed. Hypercholesterolemia. InTechOpen; 2015.
- Soran H, Durrington PN. Susceptibility of LDL and its subfractions to glycation. Curr Opin Lipidol. 2011;22(4):254-261.
- Fisher EA, Feig JE, Hewing B, Hazen SL, Smith JD. High-density lipoprotein function, dysfunction, and reverse cholesterol transport. Arteriosclerosis, thrombosis, and vascular biology. 2012;32(12):2813-2820.
- Bansal S, Buring JE, Rifai N, Mora S, Sacks FM, Ridker PM. Fasting compared with nonfasting triglycerides and risk of cardiovascular events in women. Jama. 2007;298(3):309-316.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2019;73(24):e285-e350.
- Zulyniak MA, Roke K, Gerling C, Logan SL, Spriet LL, Mutch DM. Fish oil regulates blood fatty acid composition and oxylipin levels in healthy humans: A comparison of young and older men. Mol Nutr Food Res. 2016;60(3):631-641.
- Fabbrini E, Mohammed BS, Korenblat KM, et al. Effect of Fenofibrate and Niacin on Intrahepatic Triglyceride Content, Very Low-Density Lipoprotein Kinetics, and Insulin Action in Obese Subjects with Nonalcoholic Fatty Liver Disease. The Journal of Clinical Endocrinology & Metabolism. 2010;95(6):2727-2735.
- Ahmad RS, Butt MS, Sultan MT, et al. Preventive role of green tea catechins from obesity and related disorders especially hypercholesterolemia and hyperglycemia. Journal of translational medicine. 2015;13(1):79.
- Ijaz MU, Ahmed MI, Zou X, et al. Beef, Casein, and Soy Proteins Differentially Affect Lipid Metabolism, Triglycerides Accumulation and Gut Microbiota of High-Fat Diet-Fed C57BL/6J Mice. Frontiers in Microbiology. 2018;9(2200).
- Sathyapalan T, Javed Z, Rigby AS, Kilpatrick ES, Atkin SL. Soy Protein Improves Cardiovascular Risk in Subclinical Hypothyroidism: A Randomized Double-Blinded Crossover Study. Journal of the Endocrine Society. 2017;1(5):423-430.
- National Heart L, and Blood Institute (US);. ational High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. In: Blood Pressure and Cardiovascular Risk. Bethesda MD.2004.
- Health NIo. SPRINT. https://www.sprinttrial.org/public/dspHome.cfm. Published 2016. Accessed.
- Wright JT, Jr., Williamson JD, Whelton PK, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. The New England journal of medicine. 2015;373(22):2103-2116.
- Juraschek SP, Guallar E, Appel LJ, Miller ER, 3rd. Effects of vitamin C supplementation on blood pressure: a meta-analysis of randomized controlled trials. The American journal of clinical nutrition. 2012;95(5):1079-1088.
- Varshney R, Budoff MJ. Garlic and Heart Disease. The Journal of Nutrition. 2016;146(2):416S-421S.
- Xun P, Hou N, Daviglus M, et al. Fish oil, selenium and mercury in relation to incidence of hypertension: a 20-year follow-up study. Journal of Internal Medicine. 2011;270(2):175-186.
- Yang Y-K, Wang L-P, Chen L, et al. Coenzyme Q10 treatment of cardiovascular disorders of ageing including heart failure, hypertension and endothelial dysfunction. Clinica Chimica Acta. 2015;450:83-89.
- Bjornholt JV, Erikssen G, Aaser E, et al. Fasting blood glucose: an underestimated risk factor for cardiovascular death. Results from a 22-year follow-up of healthy nondiabetic men. Diabetes Care. 1999;22(1):45-49.
- Strain WD, Paldanius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol. 2018;17(1):57.
- Diseases TNIoDaDaK. Insulin Resistance & Prediabetes. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance. Published 2018. Accessed October 28, 2019.
- Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ (Clinical research ed). 2006;332(7533):73-78.
- Sood N, Baker WL, Coleman CI. Effect of glucomannan on plasma lipid and glucose concentrations, body weight, and blood pressure: systematic review and meta-analysis. Am J Clin Nutr. 2008;88(4):1167-1175.
- Kleefstra N, Bilo HJ, Bakker SJ, Houweling ST. [Chromium and insulin resistance]. Nederlands tijdschrift voor geneeskunde. 2004;148(5):217-220.
- Galloway SD, Craig TP, Cleland SJ. Effects of oral L-carnitine supplementation on insulin sensitivity indices in response to glucose feeding in lean and overweight/obese males. Amino Acids. 2011;41(2):507-515.
- Khan A, Safdar M, Ali Khan MM, Khattak KN, Anderson RA. Cinnamon Improves Glucose and Lipids of People With Type 2 Diabetes. Diabetes Care. 2003;26(12):3215.
- Georgoulis M, Kontogianni MD, Yiannakouris N. Mediterranean diet and diabetes: prevention and treatment. Nutrients. 2014;6(4):1406-1423.
- Tonetti MS, Van Dyke TE, Working group 1 of the joint EFPAAPw. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. Journal of clinical periodontology. 2013;40 Suppl 14:S24-29.
- D'Aiuto F, Orlandi M, Gunsolley JC. Evidence that periodontal treatment improves biomarkers and CVD outcomes. Journal of clinical periodontology. 2013;40 Suppl 14:S85-105.
- Rosenfeld ME. Inflammation and atherosclerosis: direct versus indirect mechanisms. Current opinion in pharmacology. 2013;13(2):154-160.
- Shreiner AB, Kao JY, Young VB. The gut microbiome in health and in disease. Current opinion in gastroenterology. 2015;31(1):69-75.
- Ma J, Li H. The Role of Gut Microbiota in Atherosclerosis and Hypertension. Frontiers in pharmacology. 2018;9:1082.
- Jones ML, Martoni CJ, Di Pietro E, Simon RR, Prakash S. Evaluation of clinical safety and tolerance of a Lactobacillus reuteri NCIMB 30242 supplement capsule: a randomized control trial. Regulatory toxicology and pharmacology : RTP. 2012;63(2):313-320.
- Jones ML, Martoni CJ, Parent M, Prakash S. Cholesterol-lowering efficacy of a microencapsulated bile salt hydrolase-active Lactobacillus reuteri NCIMB 30242 yoghurt formulation in hypercholesterolaemic adults. The British journal of nutrition. 2012;107(10):1505-1513.
- Jones ML, Martoni CJ, Prakash S. Cholesterol lowering and inhibition of sterol absorption by Lactobacillus reuteri NCIMB 30242: a randomized controlled trial. European journal of clinical nutrition. 2012;66(11):1234-1241.
- Jones ML, Martoni CJ, Tamber S, Parent M, Prakash S. Evaluation of safety and tolerance of microencapsulated Lactobacillus reuteri NCIMB 30242 in a yogurt formulation: a randomized, placebo-controlled, double-blind study. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2012;50(6):2216-2223.
- Martoni CJ, Labbe A, Ganopolsky JG, Prakash S, Jones ML. Changes in bile acids, FGF-19 and sterol absorption in response to bile salt hydrolase active L. reuteri NCIMB 30242. Gut Microbes. 2015;6(1):57-65.
- Center UoRM. Hormones and the Endocrine System. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=P00402. Published 2019. Accessed.
- Wildman RP, Colvin AB, Powell LH, et al. Associations of endogenous sex hormones with the vasculature in menopausal women: the Study of Women's Health Across the Nation (SWAN). Menopause (New York, NY). 2008;15(3):414-421.
- Publishing HH. Sex hormones and your hear. https://www.health.harvard.edu/heart-health/sex-hormones-and-your-heart. Published 2019. Accessed.
- Publishing HH. Testosterone — What It Does And Doesn't Do. https://www.health.harvard.edu/drugs-and-medications/testosterone--what-it-does-and-doesnt-do. Published 2015. Accessed December 1, 2019.
- Goodale T, Sadhu A, Petak S, Robbins R. Testosterone and the Heart. Methodist DeBakey cardiovascular journal. 2017;13(2):68-72.
- Corona G, Rastrelli G, Di Pasquale G, Sforza A, Mannucci E, Maggi M. Testosterone and Cardiovascular Risk: Meta-Analysis of Interventional Studies. J Sex Med. 2018;15(6):820-838.
- Cattabiani C, Basaria, S., Ceda, G.P. et al. . Relationship between testosterone deficiency and cardiovascular risk and mortality in adult men. J Endocrinol Invest. 2012;35.
- Malkin CJ, Pugh PJ, Morris PD, Asif S, Jones TH, Channer KS. Low serum testosterone and increased mortality in men with coronary heart disease. Heart. 2010;96(22):1821-1825.
- Mohamad MJ, Mohammad MA, Karayyem M, Hairi A, Hader AA. Serum levels of sex hormones in men with acute myocardial infarction. Neuro endocrinology letters. 2007;28(2):182-186.
- Tivesten A, Vandenput L, Carlzon D, et al. Dehydroepiandrosterone and its sulfate predict the 5-year risk of coronary heart disease events in elderly men. J Am Coll Cardiol. 2014;64(17):1801-1810.
- Budoff MJ, Ellenberg SS, Lewis CE, et al. Testosterone Treatment and Coronary Artery Plaque Volume in Older Men With Low Testosterone. Jama. 2017;317(7):708-716.
- Shaikh K, Ellenberg SS, Nakanishi R, et al. Biomarkers and Non-Calcified Coronary Artery Plaque Progression in Older Men Treated with Testosterone. The Journal of clinical endocrinology and metabolism. 2019:dgz242.
- Khosla S, Melton LJ, 3rd, Riggs BL. Estrogens and bone health in men. Calcified tissue international. 2001;69(4):189-192.
- Jankowska EA, Rozentryt P, Ponikowska B, et al. Circulating Estradiol and Mortality in Men With Systolic Chronic Heart Failure. JAMA. 2009;301(18):1892-1901.
- Ärnlöv J, Pencina MJ, Amin S, et al. Endogenous Sex Hormones and Cardiovascular Disease Incidence in Men. Annals of Internal Medicine. 2006;145(3):176-184.
- Campagnoli C, Clavel-Chapelon F, Kaaks R, Peris C, Berrino F. Progestins and progesterone in hormone replacement therapy and the risk of breast cancer. J Steroid Biochem Mol Biol. 2005;96(2):95-108.
- Clinic C. Estrogen & Hormones. https://my.clevelandclinic.org/health/articles/16979-estrogen--hormones. Published 2019. Accessed2019.
- Lobo RA. Hormone-replacement therapy: current thinking. Nature Reviews Endocrinology. 2017;13(4):220-231.
- Arnson Y, Rozanski A, Gransar H, et al. HORMONE REPLACEMENT THERAPY IS ASSOCIATED WITH LESS CORONARY ATHEROSCLEROSIS AND LOWER MORTALITY. Journal of the American College of Cardiology. 2017;69(11 Supplement):1408.
- Schierbeck LL, Rejnmark L, Tofteng CL, et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ : British Medical Journal. 2012;345:e6409.
- Zhao D, Guallar E, Ouyang P, et al. Endogenous Sex Hormones and Incident Cardiovascular Disease in Post-Menopausal Women. Journal of the American College of Cardiology. 2018;71(22):2555.
- Cannon RO. Role of nitric oxide in cardiovascular disease: focus on the endothelium. Clinical chemistry. 1998;44(8):1809.
- Naseem KM. The role of nitric oxide in cardiovascular diseases. Molecular aspects of medicine. 2005;26(1):33-65.
- Sverdlov AL, Ngo DTM, Chan WPA, Chirkov YY, Horowitz JD. Aging of the Nitric Oxide System: Are We as Old as Our NO? Journal of the American Heart Association. 2014;3(4):e000973.
- Mabuchi H, Higashikata T, Kawashiri M, et al. Reduction of serum ubiquinol-10 and ubiquinone-10 levels by atorvastatin in hypercholesterolemic patients. Journal of atherosclerosis and thrombosis. 2005;12(2):111-119.
- von Haehling S, Anker SD, Bassenge E. Statins and the role of nitric oxide in chronic heart failure. Heart failure reviews. 2003;8(1):99-106.
- Böger RH, Bode-Böger SM, Frölich JC. The l-arginine—nitric oxide pathway: role in atherosclerosis and therapeutic implications. Atherosclerosis. 1996;127(1):1-11.
- Danesi F, Ferguson LR. Could Pomegranate Juice Help in the Control of Inflammatory Diseases? Nutrients. 2017;9(9).
- Guthikonda S, Haynes WG. Homocysteine: role and implications in atherosclerosis. Curr Atheroscler Rep. 2006;8(2):100-106.
- Sun A, Chen H-M, Cheng S-J, et al. Significant association of deficiencies of hemoglobin, iron, vitamin B12, and folic acid and high homocysteine level with recurrent aphthous stomatitis. Journal of Oral Pathology & Medicine. 2015;44(4):300-305.
- Miller JW, Green R, Mungas DM, Reed BR, Jagust WJ. Homocysteine, vitamin B6, and vascular disease in AD patients. Neurology. 2002;58(10):1471-1475.
- McRae MP. Betaine supplementation decreases plasma homocysteine in healthy adult participants: a meta-analysis. Journal of chiropractic medicine. 2013;12(1):20-25.
- Administration USFaD. FDA Announces New Qualified Health Claims for EPA and DHA Omega-3 Consumption and the Risk of Hypertension and Coronary Heart Disease. https://www.fda.gov/food/cfsan-constituent-updates/fda-announces-new-qualified-health-claims-epa-and-dha-omega-3-consumption-and-risk-hypertension-and. Published 2019. Accessed October 28, 2019.
- Swanson D, Block R, Mousa SA. Omega-3 fatty acids EPA and DHA: health benefits throughout life. Advances in nutrition (Bethesda, Md). 2012;3(1):1-7.
- Kassi E, Adamopoulos C, Basdra EK, Papavassiliou AG. Role of Vitamin D in Atherosclerosis. Circulation. 2013;128(23):2517-2531.
- Dobnig H, Pilz S, Scharnagl H, et al. Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008;168(12):1340-1349.
- Health NIo. Vitamin K: Fact Sheet for Health Professionals. https://ods.od.nih.gov/factsheets/vitaminK-HealthProfessional/. Published 2019. Accessed Ocotber 24, 2019.
- Plank F, Beyer C, Friedrich G, et al. Influence of vitamin K antagonists and direct oral anticoagulation on coronary artery disease: A CTA analysis. Int J Cardiol. 2018;260:11-15.
- Shea MK, O’Donnell CJ, Hoffmann U, et al. Vitamin K supplementation and progression of coronary artery calcium in older men and women. The American Journal of Clinical Nutrition. 2009;89(6):1799-1807.
- Knapen MH, Braam LA, Drummen NE, Bekers O, Hoeks AP, Vermeer C. Menaquinone-7 supplementation improves arterial stiffness in healthy postmenopausal women. A double-blind randomised clinical trial. Thrombosis and haemostasis. 2015;113(5):1135-1144.
- Mansour AG, Hariri E, Daaboul Y, et al. Vitamin K2 supplementation and arterial stiffness among renal transplant recipients-a single-arm, single-center clinical trial. Journal of the American Society of Hypertension : JASH. 2017;11(9):589-597.
- Cerit L. Fibrinogen and Atherosclerosis. Arquivos brasileiros de cardiologia. 2017;108(2):189-190.
- Liu MY, Hu DY. [The predictive value of serum advanced fibrinogen and uric acid for acute coronary event risk]. Zhonghua yi xue za zhi. 2006;86(10):678-680.
- Høstmark AT, Bjerkedal T, Kierulf P, Flaten H, Ulshagen K. Fish oil and plasma fibrinogen. BMJ (Clinical research ed). 1988;297(6642):180-181.
- Wannamethee SG, Lowe GD, Rumley A, Bruckdorfer KR, Whincup PH. Associations of vitamin C status, fruit and vegetable intakes, and markers of inflammation and hemostasis. Am J Clin Nutr. 2006;83(3):567-574; quiz 726-567.
- Weng Y, Yao J, Sparks S, Wang KY. Nattokinase: An Oral Antithrombotic Agent for the Prevention of Cardiovascular Disease. International journal of molecular sciences. 2017;18(3):523.
- Devaraj S, Xu DY, Jialal I. C-reactive protein increases plasminogen activator inhibitor-1 expression and activity in human aortic endothelial cells: implications for the metabolic syndrome and atherothrombosis. Circulation. 2003;107(3):398-404.
- Asher J, Houston M. Statins and C-reactive protein levels. Journal of clinical hypertension (Greenwich, Conn). 2007;9(8):622-628.
- Banerjee M, Tripathi LM, Srivastava VM, Puri A, Shukla R. Modulation of inflammatory mediators by ibuprofen and curcumin treatment during chronic inflammation in rat. Immunopharmacology and immunotoxicology. 2003;25(2):213-224.
- Ngondi JL, Etoundi BC, Nyangono CB, Mbofung CM, Oben JE. IGOB131, a novel seed extract of the West African plant Irvingia gabonensis, significantly reduces body weight and improves metabolic parameters in overweight humans in a randomized double-blind placebo controlled investigation. Lipids in health and disease. 2009;8:7-7.
- Biniaz V, Sadeghi Shermeh M, Ebadi A, Tayebi A, Einollahi B. Effect of Vitamin C Supplementation on C-reactive Protein Levels in Patients Undergoing Hemodialysis: A Randomized, Double Blind, Placebo-Controlled Study. Nephro-urology monthly. 2013;6(1):e13351-e13351.
- Tabrizi R, Vakili S, Akbari M, et al. The effects of curcumin-containing supplements on biomarkers of inflammation and oxidative stress: A systematic review and meta-analysis of randomized controlled trials. Phytother Res. 2019;33(2):253-262.
- Bowden RG, Wilson RL, Deike E, Gentile M. Fish oil supplementation lowers C-reactive protein levels independent of triglyceride reduction in patients with end-stage renal disease. Nutr Clin Pract. 2009;24(4):508-512.
- Reed GW, Leung K, Rossetti RG, Vanbuskirk S, Sharp JT, Zurier RB. Treatment of rheumatoid arthritis with marine and botanical oils: an 18-month, randomized, and double-blind trial. Evidence-based complementary and alternative medicine : eCAM. 2014;2014:857456-857456.
- Ma Y, Griffith JA, Chasan-Taber L, et al. Association between dietary fiber and serum C-reactive protein. The American journal of clinical nutrition. 2006;83(4):760-766.
- Vlassara H, Cai W, Crandall J, et al. Inflammatory mediators are induced by dietary glycotoxins, a major risk factor for diabetic angiopathy. Proc Natl Acad Sci U S A. 2002;99(24):15596-15601.
- Greenow K, Pearce NJ, Ramji DP. The key role of apolipoprotein E in atherosclerosis. Journal of molecular medicine (Berlin, Germany). 2005;83(5):329-342.
- Marais AD. Apolipoprotein E in lipoprotein metabolism, health and cardiovascular disease. Pathology. 2019;51(2):165-176.
- Wu D, Sharan C, Yang H, et al. Apolipoprotein E-deficient lipoproteins induce foam cell formation by downregulation of lysosomal hydrolases in macrophages. Journal of lipid research. 2007;48(12):2571-2578.
- Mahley RW. Apolipoprotein E: from cardiovascular disease to neurodegenerative disorders. Journal of molecular medicine (Berlin, Germany). 2016;94(7):739-746.
- Bouchareychas L, Raffai RL. Apolipoprotein E and Atherosclerosis: From Lipoprotein Metabolism to MicroRNA Control of Inflammation. J Cardiovasc Dev Dis. 2018;5(2).
- Targońska-Stępniak B, Majdan M. Serum amyloid A as a marker of persistent inflammation and an indicator of cardiovascular and renal involvement in patients with rheumatoid arthritis. Mediators of inflammation. 2014;2014:793628-793628.
- Johnson BD, Kip KE, Marroquin OC, et al. Serum amyloid A as a predictor of coronary artery disease and cardiovascular outcome in women: the National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation. 2004;109(6):726-732.
- Getz GS, Krishack PA, Reardon CA. Serum amyloid A and atherosclerosis. Curr Opin Lipidol. 2016;27(5):531-535.
- King VL, Thompson J, Tannock LR. Serum amyloid A in atherosclerosis. Current Opinion in Lipidology. 2011;22(4):302-307.
- Sack GH. Serum amyloid A – a review. Molecular Medicine. 2018;24(1):46.
- Aggarwal BB, Gupta SC, Sung B. Curcumin: an orally bioavailable blocker of TNF and other pro-inflammatory biomarkers. Br J Pharmacol. 2013;169(8):1672-1692.
- Silva AM, Oliveira MI, Sette L, et al. Resveratrol as a natural anti-tumor necrosis factor-alpha molecule: implications to dendritic cells and their crosstalk with mesenchymal stromal cells. PLoS One. 2014;9(3):e91406.
- Jamaluddin MS, Weakley SM, Yao Q, Chen C. Resistin: functional roles and therapeutic considerations for cardiovascular disease. Br J Pharmacol. 2012;165(3):622-632.
- Hyeong Kyu Park1 MKK, Hye Jeong Kim1, Rexford S. Ahima2. Linking resistin, inflammation, and cardiometabolic diseases FAU - Park, Hyeong Kyu FAU - Kwak, Mi Kyung FAU - Kim, Hye Jeong FAU - Ahima, Rexford S. The Korean journal of internal medicine. 2017;32(2):239-247.
- Chu S, Ding W, Li K, Pang Y, Tang C. Plasma resistin associated with myocardium injury in patients with acute coronary syndrome. Circulation journal : official journal of the Japanese Circulation Society. 2008;72(8):1249-1253.
- Bo S, Ciccone G, Durazzo M, et al. Efficacy of antioxidant treatment in reducing resistin serum levels: a randomized study. PLoS Clin Trials. 2007;2(5):e17-e17.
- Dehghani S, Alipoor E, Salimzadeh A, et al. The effect of a garlic supplement on the pro-inflammatory adipocytokines, resistin and tumor necrosis factor-alpha, and on pain severity, in overweight or obese women with knee osteoarthritis. Phytomedicine. 2018;48:70-75.
- Morioka T, Emoto M, Yamazaki Y, et al. Leptin is associated with vascular endothelial function in overweight patients with type 2 diabetes. Cardiovascular diabetology. 2014;13:10-10.
- Askari H, Tykodi G, Liu J, Dagogo-Jack S. Fasting plasma leptin level is a surrogate measure of insulin sensitivity. The Journal of clinical endocrinology and metabolism. 2010;95(8):3836-3843.
- Gijon-Conde T, Graciani A, Guallar-Castillon P, Aguilera MT, Rodriguez-Artalejo F, Banegas JR. Leptin Reference Values and Cutoffs for Identifying Cardiometabolic Abnormalities in the Spanish Population. Rev Esp Cardiol (Engl Ed). 2015;68(8):672-679.
- Ahima RS. Revisiting leptin's role in obesity and weight loss. The Journal of clinical investigation. 2008;118(7):2380-2383.
- Rubenfire M, American College of Cardiology. Lipoprotein(a): Diagnosis, Prognosis, Emerging Therapies. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/02/07/14/21/a-test-in-context-lipoproteina-diagnosis. Published 2017. Accessed Jun. 27, 2019.
- Schettler VJJ, Neumann CL, Peter C, et al. Lipoprotein apheresis is an optimal therapeutic option to reduce increased Lp(a) levels. Clinical research in cardiology supplements. 2019;14(Suppl 1):33-38.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2018:25709.
- Thanassoulis G. Screening for High Lipoprotein(a): The Time Is Now. Circulation. 2019;139(12):1493-1496.
- Borrelli MJ, Youssef A, Boffa MB, Koschinsky ML. New Frontiers in Lp(a)-Targeted Therapies. Trends Pharmacol Sci. 2019;40(3):212-225.
- Reiner Z. Can Lp(a) Lowering Against Background Statin Therapy Really Reduce Cardiovascular Risk? Curr Atheroscler Rep. 2019;21(4):14.
- Parikh P, Shah N, Ahmed H, Schoenhagen P, Fares M. Coronary artery calcium scoring: Its practicality and clinical utility in primary care. Cleveland Clinic journal of medicine. 2018;85(9):707-716.
- Okahara A, Sadamatsu K, Matsuura T, Koga Y, Mine D, Yoshida K. Coronary Artery Disease Screening With Carotid Ultrasound Examination by a Primary Care Physician. Cardiol Res. 2016;7(1):9-16.
- Genkel VV, Kuznetsova AS, Sumerkina VS, Salashenko AO, Shaposhnik, II. The prognostic value of various carotid ultrasound parameters in patients at high and very high cardiovascular risk. Int J Cardiol. 2019;292:225-229.
- Hoke M, Schillinger M, Minar E, Goliasch G, Binder CJ, Mayer FJ. Carotid ultrasound investigation as a prognostic tool for patients with diabetes mellitus. Cardiovasc Diabetol. 2019;18(1):90.
- Harvard Medical School. New ways to beat osteoarthritis pain. https://www.health.harvard.edu/pain/new-ways-to-beat-osteoarthritis-pain. Published 2013. Accessed June 27, 2019.
- DiNicolantonio JJ, O’Keefe JH. Importance of maintaining a low omega–6/omega–3 ratio for reducing inflammation. Open Heart. 2018;5(2):e000946.
- Martínez-González MA, Gea A, Ruiz-Canela M. The Mediterranean Diet and Cardiovascular Health. Circulation Research. 2019;124(5):779-798.
- Dalen JE, Devries S. Diets to prevent coronary heart disease 1957-2013: what have we learned? Am J Med. 2014;127(5):364-369.
- Ahmad S, Moorthy MV, Demler OV, et al. Assessment of Risk Factors and Biomarkers Associated With Risk of Cardiovascular Disease Among Women Consuming a Mediterranean Diet. JAMA Network Open. 2018;1(8):e185708-e185708.
- Simopoulos AP. Evolutionary Aspects of the Dietary Omega-6/Omega-3 Fatty Acid Ratio: Medical Implications. In: Alvergne A, Jenkinson C, Faurie C, eds. Evolutionary Thinking in Medicine: From Research to Policy and Practice. Cham: Springer International Publishing; 2016:119-134.
- Simopoulos AP. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2002;56(8):365-379.
- Simopoulos AP. An Increase in the Omega-6/Omega-3 Fatty Acid Ratio Increases the Risk for Obesity. Nutrients. 2016;8(3):128.
- Young DR, Hivert MF, Alhassan S, et al. Sedentary Behavior and Cardiovascular Morbidity and Mortality: A Science Advisory From the American Heart Association. Circulation. 2016;134(13):e262-279.
- Piercy KL, Troiano RP, Ballard RM, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020-2028.
- Mann S, Beedie C, Jimenez A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports medicine (Auckland, NZ). 2014;44(2):211-221.
- National Heart L, and Blood Institiute. Smoking and Your Heart. https://www.nhlbi.nih.gov/health-topics/smoking-and-your-heart. Published 2018. Accessed October 22, 2019.
- Institute of Medicine Committee on Secondhand Smoke E, Acute Coronary E. In: Secondhand Smoke Exposure and Cardiovascular Effects: Making Sense of the Evidence. Washington (DC): National Academies Press (US) Copyright 2010 by the National Academy of Sciences. All rights reserved.; 2010.
- Otsuka R, Watanabe H, Hirata K, et al. Acute effects of passive smoking on the coronary circulation in healthy young adults. JAMA. 2001;286(4):436-441.
- Kavalipati N, Shah J, Ramakrishan A, Vasnawala H. Pleiotropic effects of statins. Indian J Endocrinol Metab. 2015;19(5):554-562.
- Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315-2381.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2019;74(10):e177-e232.
- Fernandes A, McEvoy JW, Halvorsen S. "Doctor, Should I Keep Taking an Aspirin a Day?". The New England journal of medicine. 2019;380(20):1967-1970.
- Bavry AA, Elgendy IY, Elbez Y, et al. Aspirin and the risk of cardiovascular events in atherosclerosis patients with and without prior ischemic events. Clinical Cardiology. 2017;40(9):732-739.
- Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus. New England Journal of Medicine. 2018;379(16):1529-1539.
- J Michael Gaziano CB, Rosa Coppolecchia,Claudio Cricelli,Harald Darius,Philip B Gorelick,George Howard,Thomas A Pearson,Peter M Rothwell,Luis Miguel Ruilope,Michal. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. The Lanclet. 2018;392:P1036-1046.
- McNeil JJ, Woods RL, Nelson MR, et al. Effect of Aspirin on Disability-free Survival in the Healthy Elderly. New England Journal of Medicine. 2018;379(16):1499-1508.
- Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481-1486.
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493-503.
- Mulrow CD, Chiquette E, Angel L, et al. Dieting to reduce body weight for controlling hypertension in adults. The Cochrane database of systematic reviews. 2000(2):CD000484.
- Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38(5):1112-1117.
- Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ (Clinical research ed). 2013;346:f1326.
- Juraschek SP, Miller ER, 3rd, Weaver CM, Appel LJ. Effects of Sodium Reduction and the DASH Diet in Relation to Baseline Blood Pressure. Journal of the American College of Cardiology. 2017;70(23):2841-2848.
- Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. The New England journal of medicine. 2008;359(15):1577-1589.
- Zinman B, Lachin JM, Inzucchi SE. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. The New England journal of medicine. 2016;374(11):1094.
- Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. The New England journal of medicine. 2019;380(24):2295-2306.
- Verma S, Poulter NR, Bhatt DL, et al. Effects of Liraglutide on Cardiovascular Outcomes in Patients With Type 2 Diabetes Mellitus With or Without History of Myocardial Infarction or Stroke. Circulation. 2018;138(25):2884-2894.
- Sattar N, Petrie MC, Zinman B, Januzzi JL, Jr. Novel Diabetes Drugs and the Cardiovascular Specialist. Journal of the American College of Cardiology. 2017;69(21):2646-2656.
- Khan SS, Ning H, Wilkins JT, et al. Association of Body Mass Index With Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018;3(4):280-287.
- Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Journal of the American College of Cardiology. 2014;64(18):1929-1949.
- Lamas GA, Goertz C, Boineau R, et al. Effect of disodium EDTA chelation regimen on cardiovascular events in patients with previous myocardial infarction: the TACT randomized trial. Jama. 2013;309(12):1241-1250.
- Ahlbom M, Hagerman I, Ståhlberg M, et al. Increases in Cardiac Output and Oxygen Consumption During Enhanced External Counterpulsation. Heart, lung & circulation. 2016;25(11):1133-1136.
- Feldman AM, Silver MA, Francis GS, et al. Enhanced external counterpulsation improves exercise tolerance in patients with chronic heart failure. Journal of the American College of Cardiology. 2006;48(6):1198-1205.
- Rampengan SH, Prihartono J, Siagian M, Immanuel S. The Effect of Enhanced External Counterpulsation Therapy and Improvement of Functional Capacity in Chronic Heart Failure patients: a Randomized Clinical Trial. Acta medica Indonesiana. 2015;47(4):275-282.
- Beck DT, Casey DP, Martin JS, Sardina PD, Braith RW. Enhanced external counterpulsation reduces indices of central blood pressure and myocardial oxygen demand in patients with left ventricular dysfunction. Clinical and experimental pharmacology & physiology. 2015;42(4):315-320.
- Guluma KZ, Liebeskind DS, Raman R, et al. Feasibility and Safety of Using External Counterpulsation to Augment Cerebral Blood Flow in Acute Ischemic Stroke-The Counterpulsation to Upgrade Forward Flow in Stroke (CUFFS) Trial. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2015;24(11):2596-2604.
- Sardina PD, Martin JS, Avery JC, Braith RW. Enhanced external counterpulsation (EECP) improves biomarkers of glycemic control in patients with non-insulin-dependent type II diabetes mellitus for up to 3 months following treatment. Acta Diabetol. 2016;53(5):745-752.
- Sardina PD, Martin JS, Dzieza WK, Braith RW. Enhanced external counterpulsation (EECP) decreases advanced glycation end products and proinflammatory cytokines in patients with non-insulin-dependent type II diabetes mellitus for up to 6 months following treatment. Acta Diabetol. 2016;53(5):753-760.
- Tardif J-C, Kouz S, Waters DD, et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. New England Journal of Medicine. 2019.
- Yan BP, Tan G-M. What's Old is New Again - A Review of the Current Evidence of Colchicine in Cardiovascular Medicine. Current cardiology reviews. 2017;13(2):130-138.
- Alkadi H, Khubeiz MJ, Jbeily R. Colchicine: A Review on Chemical Structure and Clinical Usage. Infectious disorders drug targets. 2018;18(2):105-121.
- Angelidis C, Kotsialou Z, Kossyvakis C, et al. Colchicine Pharmacokinetics and Mechanism of Action. Current pharmaceutical design. 2018;24(6):659-663.
- Harris R, Croce B, Tian DH. Coronary artery bypass grafting. Ann Cardiothorac Surg. 2013;2(4):579.
- Maron DJ. ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). 2019 Oct 18. Identifier NCT01471522. International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA). https://clinicaltrials.gov/ct2/show/NCT01471522. Accessed 12/19/2019.
- Badimon L, Vilahur G, Padro T. Nutraceuticals and atherosclerosis: human trials. Cardiovascular therapeutics. 2010;28(4):202-215.
- Hu FB, Stampfer MJ, Manson JE, et al. Dietary fat intake and the risk of coronary heart disease in women. The New England journal of medicine. 1997;337(21):1491-1499.
- Esrey KL, Joseph L, Grover SA. Relationship between dietary intake and coronary heart disease mortality: lipid research clinics prevalence follow-up study. Journal of clinical epidemiology. 1996;49(2):211-216.
- Posner BM, Cobb JL, Belanger AJ, Cupples LA, D'Agostino RB, Stokes J, 3rd. Dietary lipid predictors of coronary heart disease in men. The Framingham Study. Arch Intern Med. 1991;151(6):1181-1187.
- Yang ZH, Gordon SM, Sviridov D, et al. Dietary supplementation with long-chain monounsaturated fatty acid isomers decreases atherosclerosis and alters lipoprotein proteomes in LDLr(-/-) mice. Atherosclerosis. 2017;262:31-38.
- Burr ML, Fehily AM, Gilbert JF, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989;2(8666):757-761.
- GISSI-Prevenzione Investigators. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto miocardico. Lancet. 1999;354(9177):447-455.
- Yokoyama M, Origasa H, Matsuzaki M, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369(9567):1090-1098.
- Zhu Y, Bo Y, Liu Y. Dietary total fat, fatty acids intake, and risk of cardiovascular disease: a dose-response meta-analysis of cohort studies. Lipids in health and disease. 2019;18(1):91.
- Hu Y, Hu FB, Manson JE. Marine Omega-3 Supplementation and Cardiovascular Disease: An Updated Meta-Analysis of 13 Randomized Controlled Trials Involving 127 477 Participants. J Am Heart Assoc. 2019;8(19):e013543.
- Tavazzi L, Maggioni AP, Marchioli R, et al. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372(9645):1223-1230.
- Siscovick DS, Barringer TA, Fretts AM, et al. Omega-3 Polyunsaturated Fatty Acid (Fish Oil) Supplementation and the Prevention of Clinical Cardiovascular Disease: A Science Advisory From the American Heart Association. Circulation. 2017;135(15):e867-e884.
- Bhatt DL. Reduce-It. Eur Heart J. 2019;40(15):1174-1175.
- Wang Q, Liang X, Wang L, et al. Effect of omega-3 fatty acids supplementation on endothelial function: a meta-analysis of randomized controlled trials. Atherosclerosis. 2012;221(2):536-543.
- Soliman GA. Dietary Fiber, Atherosclerosis, and Cardiovascular Disease. Nutrients. 2019;11(5).
- Threapleton DE, Greenwood DC, Evans CE, et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ (Clinical research ed). 2013;347:f6879.
- Nhung BT, Tuyen LD, Linh VA, et al. Rice Bran Extract Reduces the Risk of Atherosclerosis in Post-Menopausal Vietnamese Women. J Nutr Sci Vitaminol (Tokyo). 2016;62(5):295-302.
- Valls RM, Farras M, Suarez M, et al. Effects of functional olive oil enriched with its own phenolic compounds on endothelial function in hypertensive patients. A randomised controlled trial. Food Chem. 2015;167:30-35.
- Moss JW, Ramji DP. Nutraceutical therapies for atherosclerosis. Nature reviews Cardiology. 2016;13(9):513-532.
- Flammer AJ, Sudano I, Wolfrum M, et al. Cardiovascular effects of flavanol-rich chocolate in patients with heart failure. Eur Heart J. 2012;33(17):2172-2180.
- West SG, McIntyre MD, Piotrowski MJ, et al. Effects of dark chocolate and cocoa consumption on endothelial function and arterial stiffness in overweight adults. The British journal of nutrition. 2014;111(4):653-661.
- Grassi D, Mulder TP, Draijer R, Desideri G, Molhuizen HO, Ferri C. Black tea consumption dose-dependently improves flow-mediated dilation in healthy males. J Hypertens. 2009;27(4):774-781.
- D'Andrea G. Pycnogenol: a blend of procyanidins with multifaceted therapeutic applications? Fitoterapia. 2010;81(7):724-736.
- Rohdewald P. A review of the French maritime pine bark extract (Pycnogenol), a herbal medication with a diverse clinical pharmacology. International journal of clinical pharmacology and therapeutics. 2002;40(4):158-168.
- Gu JQ, Ikuyama S, Wei P, et al. Pycnogenol, an extract from French maritime pine, suppresses Toll-like receptor 4-mediated expression of adipose differentiation-related protein in macrophages. Am J Physiol Endocrinol Metab. 2008;295(6):E1390-1400.
- Enseleit F, Sudano I, Periat D, et al. Effects of Pycnogenol on endothelial function in patients with stable coronary artery disease: a double-blind, randomized, placebo-controlled, cross-over study. Eur Heart J. 2012;33(13):1589-1597.
- Casas R, Estruch R, Sacanella E. Influence of Bioactive Nutrients on the Atherosclerotic Process: A Review. Nutrients. 2018;10(11).
- Dower JI, Geleijnse JM, Gijsbers L, Schalkwijk C, Kromhout D, Hollman PC. Supplementation of the Pure Flavonoids Epicatechin and Quercetin Affects Some Biomarkers of Endothelial Dysfunction and Inflammation in (Pre)Hypertensive Adults: A Randomized Double-Blind, Placebo-Controlled, Crossover Trial. J Nutr. 2015;145(7):1459-1463.
- Berbee JF, Wong MC, Wang Y, et al. Resveratrol protects against atherosclerosis, but does not add to the antiatherogenic effect of atorvastatin, in APOE*3-Leiden.CETP mice. J Nutr Biochem. 2013;24(8):1423-1430.
- Imamura H, Yamaguchi T, Nagayama D, Saiki A, Shirai K, Tatsuno I. Resveratrol Ameliorates Arterial Stiffness Assessed by Cardio-Ankle Vascular Index in Patients With Type 2 Diabetes Mellitus. Int Heart J. 2017;58(4):577-583.
- Devi KP, Rajavel T, Nabavi SF, et al. Hesperidin: A promising anticancer agent from nature. Industrial crops and products. 2015;76:582-589.
- Umeno A, Horie M, Murotomi K, Nakajima Y, Yoshida Y. Antioxidative and Antidiabetic Effects of Natural Polyphenols and Isoflavones. Molecules (Basel, Switzerland). 2016;21(6).
- Li C, Schluesener H. Health-promoting effects of the citrus flavanone hesperidin. Crit Rev Food Sci Nutr. 2017;57(3):613-631.
- Roohbakhsh A, Parhiz H, Soltani F, Rezaee R, Iranshahi M. Molecular mechanisms behind the biological effects of hesperidin and hesperetin for the prevention of cancer and cardiovascular diseases. Life Sci. 2015;124:64-74.
- Rizza S, Muniyappa R, Iantorno M, et al. Citrus polyphenol hesperidin stimulates production of nitric oxide in endothelial cells while improving endothelial function and reducing inflammatory markers in patients with metabolic syndrome. J Clin Endocrinol Metab. 2011;96(5):E782-792.
- Vilaplana-Pérez C, Auñón D, García-Flores LA, Gil-Izquierdo A. Hydroxytyrosol and potential uses in cardiovascular diseases, cancer, and AIDS. Frontiers in nutrition. 2014;1:18-18.
- Covas MI, Nyyssonen K, Poulsen HE, et al. The effect of polyphenols in olive oil on heart disease risk factors: a randomized trial. Ann Intern Med. 2006;145(5):333-341.
- Ras RT, Fuchs D, Koppenol WP, et al. The effect of a low-fat spread with added plant sterols on vascular function markers: results of the Investigating Vascular Function Effects of Plant Sterols (INVEST) study. Am J Clin Nutr. 2015;101(4):733-741.
- Rocha VZ, Ras RT, Gagliardi AC, Mangili LC, Trautwein EA, Santos RD. Effects of phytosterols on markers of inflammation: A systematic review and meta-analysis. Atherosclerosis. 2016;248:76-83.
- Andersson SW, Skinner J, Ellegard L, et al. Intake of dietary plant sterols is inversely related to serum cholesterol concentration in men and women in the EPIC Norfolk population: a cross-sectional study. European journal of clinical nutrition. 2004;58(10):1378-1385.
- Kurano M, Hasegawa K, Kunimi M, et al. Sitosterol prevents obesity-related chronic inflammation. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2018;1863(2):191-198.
- C.O. Olaiya* TOO, A.M. Esan and Bukola J. Adediran Renal, Cardiac and Osteo – protective effects of beta – sitosterol glycoside in hypertensive rats. Advances in Life Science and Technology. 2015;39.
- Health NIo. Vitamin and Mineral Fact Sheets. https://ods.od.nih.gov/factsheets/list-VitaminsMinerals/. Published 2019. Accessed October 24, 2019.
- Choe H, Hwang J-Y, Yun JA, et al. Intake of antioxidants and B vitamins is inversely associated with ischemic stroke and cerebral atherosclerosis. Nutrition research and practice. 2016;10(5):516-523.
- Menzel D, Haller H, Wilhelm M, Robenek H. l-Arginine and B vitamins improve endothelial function in subjects with mild to moderate blood pressure elevation. European journal of nutrition. 2018;57(2):557-568.
- Health NIo. Niacin: Facts Sheets for Health Professionals. https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/. Published 2019. Accessed Ocotber 24, 2019.
- Altschul R, Hoffer A, Stephen JD. Influence of nicotinic acid on serum cholesterol in man. Archives of biochemistry and biophysics. 1955;54(2):558-559.
- Tavintharan S, Kashyap ML. The benefits of niacin in atherosclerosis. Curr Atheroscler Rep. 2001;3(1):74-82.
- Su G, Sun G, Liu H, et al. Niacin Suppresses Progression of Atherosclerosis by Inhibiting Vascular Inflammation and Apoptosis of Vascular Smooth Muscle Cells. Medical science monitor : international medical journal of experimental and clinical research. 2015;21:4081-4089.
- Villines TC, Stanek EJ, Devine PJ, et al. The ARBITER 6-HALTS Trial (Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol 6-HDL and LDL Treatment Strategies in Atherosclerosis): final results and the impact of medication adherence, dose, and treatment duration. Journal of the American College of Cardiology. 2010;55(24):2721-2726.
- Health NIo. Vitamin C Fact Sheet. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/. Published 2019. Accessed October 23, 2019.
- Health NIo. Vitamin E Fact Sheet. https://ods.od.nih.gov/factsheets/VitaminE-HealthProfessional/. Published 2019. Accessed.
- Rashidi B, Hoseini Z, Sahebkar A, Mirzaei H. Anti-Atherosclerotic Effects of Vitamins D and E in Suppression of Atherogenesis. Journal of Cellular Physiology. 2017;232(11):2968-2976.
- Myint PK, Luben RN, Welch AA, Bingham SA, Wareham NJ, Khaw KT. Plasma vitamin C concentrations predict risk of incident stroke over 10 y in 20 649 participants of the European Prospective Investigation into Cancer Norfolk prospective population study. Am J Clin Nutr. 2008;87(1):64-69.
- Salonen RM, Nyyssönen K, Kaikkonen J, et al. Six-Year Effect of Combined Vitamin C and E Supplementation on Atherosclerotic Progression. Circulation. 2003;107(7):947-953.
- Mathur P, Ding Z, Saldeen T, Mehta JL. Tocopherols in the Prevention and Treatment of Atherosclerosis and Related Cardiovascular Disease. Clinical Cardiology. 2015;38(9):570-576.
- Kurnatowska I, Grzelak P, Masajtis-Zagajewska A, et al. Effect of vitamin K2 on progression of atherosclerosis and vascular calcification in nondialyzed patients with chronic kidney disease stages 3-5. Polskie Archiwum Medycyny Wewnetrznej. 2015;125(9):631-640.
- Ghirlanda G, Oradei A, Manto A, et al. Evidence of plasma CoQ10-lowering effect by HMG-CoA reductase inhibitors: a double-blind, placebo-controlled study. J Clin Pharmacol. 1993;33(3):226-229.
- Ruiz-Leon AM, Lapuente M, Estruch R, Casas R. Clinical Advances in Immunonutrition and Atherosclerosis: A Review. Front Immunol. 2019;10:837.
- Larijani VN, Ahmadi N, Zeb I, Khan F, Flores F, Budoff M. Beneficial effects of aged garlic extract and coenzyme Q10 on vascular elasticity and endothelial function: the FAITH randomized clinical trial. Nutrition (Burbank, Los Angeles County, Calif). 2013;29(1):71-75.
- Zeb I, Ahmadi N, Nasir K, et al. Aged garlic extract and coenzyme Q10 have favorable effect on inflammatory markers and coronary atherosclerosis progression: A randomized clinical trial. Journal of cardiovascular disease research. 2012;3(3):185-190.
- Gao L, Mao Q, Cao J, Wang Y, Zhou X, Fan L. Effects of coenzyme Q10 on vascular endothelial function in humans: a meta-analysis of randomized controlled trials. Atherosclerosis. 2012;221(2):311-316.
- Yan X, Shen T, Jiang X, et al. Coenzyme Q10 consumption promotes ABCG1-mediated macrophage cholesterol efflux: a randomized, double-blind, placebo-controlled, cross-over study in healthy volunteers. Mol Nutr Food Res. 2015;59(9):1725-1734.
- Ya F, Zhang P, Tian Z, Li Q, Ling W, Yang Y. Coenzyme Q10 Reduces Platelet Hyperreactivity and Attenuates Atherosclerosis via Inhibiting Platelet αIIbβ3-mediated Signaling Pathway. Atherosclerosis Supplements. 2018;32:126-127.
- Severino P, Netti L, Mariani MV, et al. Prevention of Cardiovascular Disease: Screening for Magnesium Deficiency. Cardiology research and practice. 2019;2019:4874921-4874921.
- Purvis JR, Cummings DM, Landsman P, et al. Effect of oral magnesium supplementation on selected cardiovascular risk factors in non-insulin-dependent diabetics. Archives of family medicine. 1994;3(6):503-508.
- Cunha AR, D'El-Rei J, Medeiros F, et al. Oral magnesium supplementation improves endothelial function and attenuates subclinical atherosclerosis in thiazide-treated hypertensive women. Journal of hypertension. 2017;35(1):89-97.
- Joris PJ, Plat J, Bakker SJ, Mensink RP. Long-term magnesium supplementation improves arterial stiffness in overweight and obese adults: results of a randomized, double-blind, placebo-controlled intervention trial. Am J Clin Nutr. 2016;103(5):1260-1266.
- Tzanakis IP, Stamataki EE, Papadaki AN, Giannakis N, Damianakis NE, Oreopoulos DG. Magnesium retards the progress of the arterial calcifications in hemodialysis patients: a pilot study. International urology and nephrology. 2014;46(11):2199-2205.
- Simental-Mendia LE, Rodriguez-Moran M, Guerrero-Romero F. Oral magnesium supplementation decreases C-reactive protein levels in subjects with prediabetes and hypomagnesemia: a clinical randomized double-blind placebo-controlled trial. Arch Med Res. 2014;45(4):325-330.
- Guasch-Ferre M, Bullo M, Estruch R, et al. Dietary magnesium intake is inversely associated with mortality in adults at high cardiovascular disease risk. J Nutr. 2014;144(1):55-60.
- Spagnoli LG, Orlandi A, Marino B, Mauriello A, De Angelis C, Ramacci MT. Propionyl-L-carnitine prevents the progression of atherosclerotic lesions in aged hyperlipemic rabbits. Atherosclerosis. 1995;114(1):29-44.
- Mingorance C, Duluc L, Chalopin M, et al. Propionyl-L-carnitine corrects metabolic and cardiovascular alterations in diet-induced obese mice and improves liver respiratory chain activity. PLoS One. 2012;7(3):e34268.
- Kaiser KP, Feinendegen LE. [Planar scintigraphy versus PET in measuring fatty acid metabolism of the heart]. Herz. 1987;12(1):41-50.
- Scioli MG, Lo Giudice P, Bielli A, et al. Propionyl-L-Carnitine Enhances Wound Healing and Counteracts Microvascular Endothelial Cell Dysfunction. PloS one. 2015;10(10):e0140697-e0140697.
- Wiseman LR, Brogden RN. Propionyl-L-carnitine. Drugs Aging. 1998;12(3):243-248; discussion 249-250.
- Derave W, Everaert I, Beeckman S, Baguet A. Muscle carnosine metabolism and beta-alanine supplementation in relation to exercise and training. Sports medicine (Auckland, NZ). 2010;40(3):247-263.
- Rashid I, van Reyk DM, Davies MJ. Carnosine and its constituents inhibit glycation of low-density lipoproteins that promotes foam cell formation in vitro. FEBS letters. 2007;581(5):1067-1070.
- Baye E, Ukropcova B, Ukropec J, Hipkiss A, Aldini G, de Courten B. Physiological and therapeutic effects of carnosine on cardiometabolic risk and disease. Amino Acids. 2016;48(5):1131-1149.
- de Courten B, Jakubova M, de Courten MP, et al. Effects of carnosine supplementation on glucose metabolism: Pilot clinical trial. Obesity (Silver Spring). 2016;24(5):1027-1034.
- Packer L, Kraemer K, Rimbach G. Molecular aspects of lipoic acid in the prevention of diabetes complications. Nutrition (Burbank, Los Angeles County, Calif). 2001;17(10):888-895.
- Skibska B, Goraca A. The protective effect of lipoic acid on selected cardiovascular diseases caused by age-related oxidative stress. Oxid Med Cell Longev. 2015;2015:313021.
- Ying Z, Kherada N, Farrar B, et al. Lipoic acid effects on established atherosclerosis. Life Sci. 2010;86(3-4):95-102.
- Sola S, Mir MQ, Cheema FA, et al. Irbesartan and lipoic acid improve endothelial function and reduce markers of inflammation in the metabolic syndrome: results of the Irbesartan and Lipoic Acid in Endothelial Dysfunction (ISLAND) study. Circulation. 2005;111(3):343-348.
- Katoh A, Kai H, Harada H, Niiyama H, Ikeda H. Oral Administration of Glucosamine Improves Vascular Endothelial Function by Modulating Intracellular Redox State. Int Heart J. 2017;58(6):926-932.
- Bell GA, Kantor ED, Lampe JW, Shen DD, White E. Use of glucosamine and chondroitin in relation to mortality. European journal of epidemiology. 2012;27(8):593-603.
- Ma H, Li X, Sun D, et al. Association of habitual glucosamine use with risk of cardiovascular disease: prospective study in UK Biobank. BMJ (Clinical research ed). 2019;365:l1628.
- Health NIo. Selenium: Fact Sheet for Professionals. https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/. Published 2019. Accessed October 24, 2019.
- Liu H, Xu H, Huang K. Selenium in the prevention of atherosclerosis and its underlying mechanisms. Metallomics. 2017;9(1):21-37.
- Krohn RM, Lemaire M, Negro Silva LF, et al. High-selenium lentil diet protects against arsenic-induced atherosclerosis in a mouse model. The Journal of Nutritional Biochemistry. 2016;27:9-15.
- Mathew A, Bashir, S., De Roos, B., & Sneddon, A. . Interaction of selenium and vitamin D and its relevance to atherosclerosis. Proceedings of the Nutrition Society. 2019;78.
- Cockcroft JR. Exploring vascular benefits of endothelium-derived nitric oxide. Am J Hypertens. 2005;18(12 Pt 2):177S-183S.
- Sudar-Milovanovic E, Obradovic M, Jovanovic A, et al. Benefits of L-Arginine on Cardiovascular System. Mini Rev Med Chem. 2016;16(2):94-103.
- Ul Ain Q, Chung H, Chung JY, Choi J-H, Kim Y-H. Amelioration of atherosclerotic inflammation and plaques via endothelial adrenoceptor-targeted eNOS gene delivery using redox-sensitive polymer bearing l-arginine. Journal of Controlled Release. 2017;262:72-86.
- Brinkmann SJ, Worner EA, Buijs N, et al. The Arginine/ADMA Ratio Is Related to the Prevention of Atherosclerotic Plaques in Hypercholesterolemic Rabbits When Giving a Combined Therapy with Atorvastatine and Arginine. International journal of molecular sciences. 2015;16(6):12230-12242.
- Di Franco M, Lucchino B, Conti F, Valesini G, Spinelli FR. Asymmetric Dimethyl Arginine as a Biomarker of Atherosclerosis in Rheumatoid Arthritis. Mediators Inflamm. 2018;2018:3897295.
- Yin WH, Chen JW, Tsai C, Chiang MC, Young MS, Lin SJ. L-arginine improves endothelial function and reduces LDL oxidation in patients with stable coronary artery disease. Clin Nutr. 2005;24(6):988-997.
- Kalman DS, Feldman S, Samson A, Krieger DR. A clinical evaluation to determine the safety, pharmacokinetics, and pharmacodynamics of an inositol-stabilized arginine silicate dietary supplement in healthy adult males. Clinical pharmacology : advances and applications. 2015;7:103-109.
- Kalman D, Harvey PD, Perez Ojalvo S, Komorowski J. Randomized Prospective Double-Blind Studies to Evaluate the Cognitive Effects of Inositol-Stabilized Arginine Silicate in Healthy Physically Active Adults. Nutrients. 2016;8(11):736.
- Proctor SD, Kelly SE, Russell JC. A novel complex of arginine-silicate improves micro- and macrovascular function and inhibits glomerular sclerosis in insulin-resistant JCR:LA-cp rats. Diabetologia. 2005;48(9):1925-1932.
- Istas G, Wood E, Le Sayec M, et al. Effects of aronia berry (poly)phenols on vascular function and gut microbiota: ad double-blind randomized controlled trial. Am J Clin Nutr. 2019;110(August 2019):316-329.
- Varela CE, Fromentin E, Roller M, Villarreal F, Ramirez-Sanchez I. Effects of a natural extract of Aronia Melanocarpa berry on endothelial cell nitric oxide production. Journal of food biochemistry. 2016;40(4):404-410.
- Banach M, Patti AM, Giglio RV, et al. The Role of Nutraceuticals in Statin Intolerant Patients. Journal of the American College of Cardiology. 2018;72(1):96-118.
- Lu Z, Kou W, Du B, et al. Effect of Xuezhikang, an extract from red yeast Chinese rice, on coronary events in a Chinese population with previous myocardial infarction. The American journal of cardiology. 2008;101(12):1689-1693.
- Kasliwal RR, Bansal M, Gupta R, et al. ESSENS dyslipidemia: A placebo-controlled, randomized study of a nutritional supplement containing red yeast rice in subjects with newly diagnosed dyslipidemia. Nutrition (Burbank, Los Angeles County, Calif). 2016;32(7-8):767-776.
- Dong Y, Cheng H, Liu Y, Xue M, Liang H. Red yeast rice ameliorates high-fat diet-induced atherosclerosis in Apoe(-/-) mice in association with improved inflammation and altered gut microbiota composition. Food Funct. 2019;10(7):3880-3889.
- Borek C. Antioxidant health effects of aged garlic extract. J Nutr. 2001;131(3s):1010S-1015S.
- Koscielny J, Klussendorf D, Latza R, et al. The antiatherosclerotic effect of Allium sativum. Atherosclerosis. 1999;144(1):237-249.
- Akazawa N, Choi Y, Miyaki A, et al. Curcumin ingestion and exercise training improve vascular endothelial function in postmenopausal women. Nutr Res. 2012;32(10):795-799.
- Meng N, Gong Y, Zhang J, et al. A novel curcumin-loaded nanoparticle restricts atherosclerosis development and promotes plaques stability in apolipoprotein E deficient mice. Journal of Biomaterials Applications. 2018;33(7):946-954.
- Chuengsamarn S, Rattanamongkolgul S, Phonrat B, Tungtrongchitr R, Jirawatnotai S. Reduction of atherogenic risk in patients with type 2 diabetes by curcuminoid extract: a randomized controlled trial. J Nutr Biochem. 2014;25(2):144-150.
- Palozza P, Parrone N, Simone RE, Catalano A. Lycopene in atherosclerosis prevention: an integrated scheme of the potential mechanisms of action from cell culture studies. Archives of biochemistry and biophysics. 2010;504(1):26-33.
- Gajendragadkar PR, Hubsch A, Maki-Petaja KM, Serg M, Wilkinson IB, Cheriyan J. Effects of oral lycopene supplementation on vascular function in patients with cardiovascular disease and healthy volunteers: a randomised controlled trial. PLoS One. 2014;9(6):e99070.
- Zeng YC, Peng LS, Zou L, et al. Protective effect and mechanism of lycopene on endothelial progenitor cells (EPCs) from type 2 diabetes mellitus rats. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2017;92:86-94.
- Tsui PF, Lin CS, Ho LJ, Lai JH. Spices and Atherosclerosis. Nutrients. 2018;10(11).
- Shemshian M, Mousavi SH, Norouzy A, et al. Saffron in metabolic syndrome: its effects on antibody titers to heat-shock proteins 27, 60, 65 and 70. Journal of complementary & integrative medicine. 2014;11(1):43-49.
- Wick G, Jakic B, Buszko M, Wick MC, Grundtman C. The role of heat shock proteins in atherosclerosis. Nature reviews Cardiology. 2014;11(9):516-529.
- Ahmadi Khatir S, Bayatian A, Barzegari A, et al. Saffron (Crocus sativus L.) Supplements Modulate Circulating MicroRNA (miR-21) in Atherosclerosis Patients; A Randomized, Double-Blind, Placebo-Controlled Trial. Iran Red Crescent Med J. 2018;20(10):e80260.
- McCarty MF, DiNicolantonio JJ, O'Keefe JH. Capsaicin may have important potential for promoting vascular and metabolic health. Open Heart. 2015;2(1):e000262.
- Fragasso G, Palloshi A, Piatti PM, et al. Nitric-oxide mediated effects of transdermal capsaicin patches on the ischemic threshold in patients with stable coronary disease. Journal of cardiovascular pharmacology. 2004;44(3):340-347.
- Qin Y, Ran L, Wang J, et al. Capsaicin Supplementation Improved Risk Factors of Coronary Heart Disease in Individuals with Low HDL-C Levels. Nutrients. 2017;9(9).
- Yang S, Liu L, Meng L, Hu X. Capsaicin is beneficial to hyperlipidemia, oxidative stress, endothelial dysfunction, and atherosclerosis in Guinea pigs fed on a high-fat diet. Chemico-Biological Interactions. 2019;297:1-7.
- Gohil KJ, Patel JA, Gajjar AK. Pharmacological Review on Centella asiatica: A Potential Herbal Cure-all. Indian J Pharm Sci. 2010;72(5):546-556.
- Incandela L, Belcaro G, Nicolaides AN, et al. Modification of the echogenicity of femoral plaques after treatment with total triterpenic fraction of Centella asiatica: a prospective, randomized, placebo-controlled trial. Angiology. 2001;52 Suppl 2:S69-73.
- Belcaro G, Maquart FX, Scoccianti M, et al. TECA (Titrated Extract of Centella Asiatica): new microcirculatory, biomolecular, and vascular application in preventive and clinical medicine. A status paper. Panminerva medica. 2011;53(3 Suppl 1):105-118.
- Cesarone MR, Belcaro G, Nicolaides AN, et al. Increase in echogenicity of echolucent carotid plaques after treatment with total triterpenic fraction of Centella asiatica: a prospective, placebo-controlled, randomized trial. Angiology. 2001;52 Suppl 2:S19-25.
- Belcaro G, Dugall M, Ippolito E, et al. Pycnogenol(R) and Centella asiatica to prevent asymptomatic atherosclerosis progression in clinical events. Minerva cardioangiologica. 2017;65(1):24-31.
- Zhiming Shu AHS, Mohamed Shahen, He Wang, Mahmoud Alagawany, Mohamed E. Abd El-Hack, Shahmir Ali Kalhoro, Muhammad Rashid and Piar Ali Shar. Pharmacological Uses of Ginkgo biloba Extracts for Cardiovascular Disease and Coronary Heart Diseases. International Journal of Pharmacology,.15:1-9.
- Kudolo GB, Wang W, Dorsey S, Blodgett J. Oral ingestion of Ginkgo biloba extract reduces thiobarbituric acid reacting (TBAR) substances in washed platelets of healthy subjects. Journal of herbal pharmacotherapy. 2003;3(4):1-15.
- Ou HC, Lee WJ, Lee IT, et al. Ginkgo biloba extract attenuates oxLDL-induced oxidative functional damages in endothelial cells. J Appl Physiol (1985). 2009;106(5):1674-1685.
- Pierre SV, Lesnik P, Moreau M, et al. The standardized Ginkgo biloba extract Egb-761 protects vascular endothelium exposed to oxidized low density lipoproteins. Cellular and molecular biology (Noisy-le-Grand, France). 2008;54 Suppl:OL1032-1042.
- Rodriguez M, Ringstad L, Schafer P, et al. Reduction of atherosclerotic nanoplaque formation and size by Ginkgo biloba (EGb 761) in cardiovascular high-risk patients. Atherosclerosis. 2007;192(2):438-444.
- Pittler MH, Ernst E. Ginkgo biloba extract for the treatment of intermittent claudication: a meta-analysis of randomized trials. Am J Med. 2000;108(4):276-281.
- Nam D-E, Yun J-M, Kim D, Kim O-K. Policosanol Attenuates Cholesterol Synthesis via AMPK Activation in Hypercholesterolemic Rats. Journal of medicinal food. 2019.
- Kim S-J, Cho K-H. Blood Pressure Lowering Effect of Cuban Policosanol is Accompanied by Improved Lipoprotein Profile, and HDL Quality in Spontaneously Hypertensive Rats. Atherosclerosis Supplements. 2018;32:128.
- Castano G, Mas R, Fernandez JC, Fernandez L, Illnait J, Lopez E. Effects of policosanol on older patients with hypertension and type II hypercholesterolaemia. Drugs in R&D. 2002;3(3):159-172.
- Center MSKC. Guggul. https://www.mskcc.org/cancer-care/integrative-medicine/herbs/guggul. Published 2018. Accessed October 24, 2019.
- Das S, Datta A, Bagchi C, Chakraborty S, Mitra A, Tripathi SK. A Comparative Study of Lipid-Lowering Effects of Guggul and Atorvastatin Monotherapy in Comparison to Their Combination in High Cholesterol Diet-Induced Hyperlipidemia in Rabbits. Journal of dietary supplements. 2016;13(5):495-504.
- Amato A, Caldara GF, Nuzzo D, et al. NAFLD and Atherosclerosis Are Prevented by a Natural Dietary Supplement Containing Curcumin, Silymarin, Guggul, Chlorogenic Acid and Inulin in Mice Fed a High-Fat Diet. Nutrients. 2017;9(5).
- Kuppurajan K, Rajagopalan SS, Rao TK, Sitaraman R. Effect of guggulu (Commiphora mukul--Engl.) on serum lipids in obese, hypercholesterolemic and hyperlipemic cases. J Assoc Physicians India. 1978;26(5):367-373.
- Medicine NCfCaI. Hawthorn. https://nccih.nih.gov/health/hawthorn. Published 2016. Accessed October 24, 2019.
- Wang S-z, Wu M, Chen K-j, et al. Hawthorn Extract Alleviates Atherosclerosis through Regulating Inflammation and Apoptosis Related Factors: An Experimental Study. Chinese journal of integrative medicine. 2019;25(2):108-115.
- Dong P, Pan L, Zhang X, et al. Hawthorn (Crataegus pinnatifida Bunge) leave flavonoids attenuate atherosclerosis development in apoE knock-out mice. Journal of ethnopharmacology. 2017;198:479-488.
- Health NIo. Potassium: Fact Sheet for Professionals. https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/. Published 2019. Accessed October 24, 2019.
- Sun Y, Byon CH, Yang Y, et al. Dietary potassium regulates vascular calcification and arterial stiffness. JCI insight. 2017;2(19).
- American Heart Association. Monounsaturated Fat. 6/1/2015. Accessed 6/5/2020. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/monounsaturated-fats.
- American Heart Association. Polyunsaturated Fat. 6/1/2015. Accessed 6/5/2020. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/polyunsaturated-fats.
- USDA. United States Department of Agriculture. FoodData Central Search Results. Olive oil. 10/28/2022. Accessed 11/4/2022.https://fdc.nal.usda.gov/fdc-app.html#/food-details/2345743/nutrients
- Gaforio JJ, Visioli F, Alarcón-de-la-Lastra C, et al. Virgin Olive Oil and Health: Summary of the III International Conference on Virgin Olive Oil and Health Consensus Report, JAEN (Spain) 2018. Nutrients. 2019;11(9):2039.
- Román GC, Jackson RE, Reis J, Román AN, Toledo JB, Toledo E. Extra-virgin olive oil for potential prevention of Alzheimer disease. Revue neurologique. 2019;175(10):705-723.
- Rigacci S, Stefani M. Nutraceutical Properties of Olive Oil Polyphenols. An Itinerary from Cultured Cells through Animal Models to Humans. International journal of molecular sciences. 2016;17(6):843.
- Saibandith B, Spencer JPE, Rowland IR, Commane DM. Olive Polyphenols and the Metabolic Syndrome. Molecules (Basel, Switzerland). 2017;22(7).
- Nocella C, Cammisotto V, Fianchini L, et al. Extra Virgin Olive Oil and Cardiovascular Diseases: Benefits for Human Health. Endocr Metab Immune Disord Drug Targets. 2018;18(1):4-13.
- Casas R, Estruch R, Sacanella E. The Protective Effects of Extra Virgin Olive Oil on Immune-mediated Inflammatory Responses. Endocr Metab Immune Disord Drug Targets. 2018;18(1):23-35.
- Farràs M, Canyelles M, Fitó M, Escolà-Gil JC. Effects of Virgin Olive Oil and Phenol-Enriched Virgin Olive Oils on Lipoprotein Atherogenicity. Nutrients. 2020;12(3):601.
- Guasch-Ferré M, Liu G, Li Y, et al. Olive Oil Consumption and Cardiovascular Risk in U.S. Adults. Journal of the American College of Cardiology. 2020;75(15):1729-1739.
- Estruch R, Ros E, Salas-Salvado J, et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. The New England journal of medicine. 2018;378(25):e34.
- Reduction of Revascularizations in Patients with Hypertriglyceridemia With Icosapent Ethyl: Insights From REDUCE-IT REVASC [press release]. Society for Cardiovascular Angiography and Interventions.2020.
- Linus Pauling Institute. Vitamin K. Published by https://lpi.oregonstate.edu/mic/vitamins/vitamin-K Updated Accessed 6/11/19.
- Shea MK, Barger K, Booth SL, et al. Vitamin K status, cardiovascular disease, and all-cause mortality: a participant-level meta-analysis of 3 US cohorts. The American journal of clinical nutrition. 2020;111(6):1170-1177.
- O'Keefe JH, Torres-Acosta N, O'Keefe EL, et al. A Pesco-Mediterranean Diet With Intermittent Fasting: JACC Review Topic of the Week. Journal of the American College of Cardiology. Sep 22 2020;76(12):1484-1493. doi:10.1016/j.jacc.2020.07.049
- Tong TYN, Appleby PN, Bradbury KE, et al. Risks of ischaemic heart disease and stroke in meat eaters, fish eaters, and vegetarians over 18 years of follow-up: results from the prospective EPIC-Oxford study. BMJ (Clinical research ed). Sep 4 2019;366:l4897. doi:10.1136/bmj.l4897
- Rynders CA, Thomas EA, Zaman A, Pan Z, Catenacci VA, Melanson EL. Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss. Nutrients. Oct 14 2019;11(10):2442. doi:10.3390/nu11102442
- Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell metabolism. Jun 5 2018;27(6):1212-1221 e3. doi:10.1016/j.cmet.2018.04.010
- Regmi P, Heilbronn LK. Time-Restricted Eating: Benefits, Mechanisms, and Challenges in Translation. iScience. 2020;23(6)doi:10.1016/j.isci.2020.101161
- Harvie M, Howell A. Potential Benefits and Harms of Intermittent Energy Restriction and Intermittent Fasting Amongst Obese, Overweight and Normal Weight Subjects-A Narrative Review of Human and Animal Evidence. Behavioral sciences (Basel, Switzerland). Jan 19 2017;7(1)doi:10.3390/bs7010004
- Lowe DA, Wu N, Rohdin-Bibby L, et al. Effects of Time-Restricted Eating on Weight Loss and Other Metabolic Parameters in Women and Men With Overweight and Obesity: The TREAT Randomized Clinical Trial. JAMA Internal Medicine. 2020;doi:10.1001/jamainternmed.2020.4153
- Bernasconi AA, Wiest MM, Lavie CJ, Milani RV, Laukkanen JA. Effect of Omega-3 Dosage on Cardiovascular Outcomes: An Updated Meta-Analysis and Meta-Regression of Interventional Trials. Mayo Clinic Proceedings. doi:10.1016/j.mayocp.2020.08.034
- McDermott MM, Spring B, Tian L, et al. Effect of Low-Intensity vs High-Intensity Home-Based Walking Exercise on Walk Distance in Patients With Peripheral Artery Disease: The LITE Randomized Clinical Trial. Jama. Apr 6 2021;325(13):1266-1276. doi:10.1001/jama.2021.2536
- Li H, Chen A, Zhao L, et al. Effect of tomato consumption on fasting blood glucose and lipid profiles: A systematic review and meta-analysis of randomized controlled trials. https://doi.org/10.1002/ptr.6660. Phytotherapy Research. 2020/08/01 2020;34(8):1956-1965. doi:https://doi.org/10.1002/ptr.6660
- Xie Z, Yang F. The effects of lycopene supplementation on serum insulin-like growth factor 1 (IGF-1) levels and cardiovascular disease: A dose-response meta-analysis of clinical trials. Complementary therapies in medicine. Jan 2021;56:102632. doi:10.1016/j.ctim.2020.102632
- Huang Y, Chen H, Su Y, Liu H, Hu J, Hong K. Increased blood alpha-carotene, all-trans-Beta-carotene and lycopene levels are associated with beneficial changes in heart rate variability: a CVD-stratified analysis in an adult population-based study. Nutr J. May 11 2021;20(1):43. doi:10.1186/s12937-021-00700-w
- Higdon J, Drake VJ, Delage B. Carotenoids: α-Carotene, β-Carotene, β-Cryptoxanthin, Lycopene, Lutein, and Zeaxanthin. Linus Pauling Institute. Updated 7/2016. Accessed 5/18/2021, https://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals/carotenoids
- Matsumoto M, Suganuma H, Ozato N, et al. Association between Serum Concentration of Carotenoid and Visceral Fat. Nutrients. Mar 11 2021;13(3)doi:10.3390/nu13030912
- Hajizadeh-Sharafabad F, Ghoreishi Z, Maleki V, Tarighat-Esfanjani A. Mechanistic insights into the effect of lutein on atherosclerosis, vascular dysfunction, and related risk factors: A systematic review of in vivo, ex vivo and in vitro studies. Pharmacological research : the official journal of the Italian Pharmacological Society. Nov 2019;149:104477. doi:10.1016/j.phrs.2019.104477
- Chung RWS, Leanderson P, Lundberg AK, Jonasson L. Lutein exerts anti-inflammatory effects in patients with coronary artery disease. Atherosclerosis. Jul 2017;262:87-93. doi:10.1016/j.atherosclerosis.2017.05.008
- Leermakers ET, Darweesh SK, Baena CP, et al. The effects of lutein on cardiometabolic health across the life course: a systematic review and meta-analysis. Am J Clin Nutr. Feb 2016;103(2):481-94. doi:10.3945/ajcn.115.120931
- Ouyang B, Li Z, Ji X, Huang J, Zhang H, Jiang C. The protective role of lutein on isoproterenol-induced cardiac failure rat model through improving cardiac morphology, antioxidant status via positively regulating Nrf2/HO-1 signalling pathway. Pharmaceutical biology. Dec 2019;57(1):529-535. doi:10.1080/13880209.2019.1649436
- Yang S, Li X, Yang F, et al. Gut Microbiota-Dependent Marker TMAO in Promoting Cardiovascular Disease: Inflammation Mechanism, Clinical Prognostic, and Potential as a Therapeutic Target. Frontiers in pharmacology. 2019;10:1360. doi:10.3389/fphar.2019.01360
- Supplements NIoHOoD. Carnitine Fact Sheet for Health Professionals. October 26, 2021. https://ods.od.nih.gov/factsheets/Carnitine-HealthProfessional/
- Craig SA. Betaine in human nutrition. The American Journal of Clinical Nutrition. 2004;80(3):539-549. doi:10.1093/ajcn/80.3.539
- Ussher JR, Lopaschuk GD, Arduini A. Gut microbiota metabolism of L-carnitine and cardiovascular risk. Atherosclerosis. Dec 2013;231(2):456-61. doi:10.1016/j.atherosclerosis.2013.10.013
- Ufnal M, Zadlo A, Ostaszewski R. TMAO: A small molecule of great expectations. Nutrition (Burbank, Los Angeles County, Calif). 2015;31(11-12):1317-1323.
- Nowiński A, Ufnal M. Trimethylamine N-oxide: A harmful, protective or diagnostic marker in lifestyle diseases? Nutrition (Burbank, Los Angeles County, Calif). Feb 2018;46:7-12. doi:10.1016/j.nut.2017.08.001
- Kim Y, Keogh J, Clifton P. A review of potential metabolic etiologies of the observed association between red meat consumption and development of type 2 diabetes mellitus. Metabolism: clinical and experimental. Jul 2015;64(7):768-79. doi:10.1016/j.metabol.2015.03.008
- Tang WW, Wang Z, Kennedy DJ, et al. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circulation research. 2015;116(3):448-455.
- Gruppen EG, Garcia E, Connelly MA, et al. TMAO is associated with mortality: impact of modestly impaired renal function. Scientific reports. 2017;7(1):1-9.
- Dehghan P, Farhangi MA, Nikniaz L, Nikniaz Z, Asghari‐Jafarabadi M. Gut microbiota‐derived metabolite trimethylamine N‐oxide (TMAO) potentially increases the risk of obesity in adults: An exploratory systematic review and dose‐response meta‐analysis. Obesity Reviews. 2020;21(5):e12993.
- Thomas MS, Fernandez ML. Trimethylamine N-Oxide (TMAO), Diet and Cardiovascular Disease. Curr Atheroscler Rep. Feb 17 2021;23(4):12. doi:10.1007/s11883-021-00910-x
- Randrianarisoa E, Lehn-Stefan A, Wang X, et al. Relationship of serum trimethylamine N-oxide (TMAO) levels with early atherosclerosis in humans. Scientific reports. 2016;6(1):1-9.
- Xu R, Wang Q, Li L. A genome-wide systems analysis reveals strong link between colorectal cancer and trimethylamine N-oxide (TMAO), a gut microbial metabolite of dietary meat and fat. BMC genomics. 2015;16(7):1-9.
- Hong Wilson Tang W, Wang Z, Wu Y, Fan Y, Koeth RA, Hazen S. Gut flora metabolite trimethylamine N-oxide predicts incident cardiovascular risks in both stable non-diabetics and diabetic subjects. Journal of the American College of Cardiology. 2013;61(10S):E1398-E1398.
- Zhang Y, Wang Y, Ke B, Du J. TMAO: how gut microbiota contributes to heart failure. Translational Research. 2021;228:109-125.
- Liu Y, Dai M. Trimethylamine N-oxide generated by the gut microbiota is associated with vascular inflammation: new insights into atherosclerosis. Mediators of inflammation. 2020;2020
- Velasquez MT, Ramezani A, Manal A, Raj DS. Trimethylamine N-Oxide: The Good, the Bad and the Unknown. Toxins. Nov 8 2016;8(11)doi:10.3390/toxins8110326
- Cho CE, Taesuwan S, Malysheva OV, et al. Trimethylamine‐N‐oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: a randomized controlled trial. Molecular nutrition & food research. 2017;61(1):1600324.
- Costabile G, Vetrani C, Bozzetto L, et al. Plasma TMAO increase after healthy diets: results from 2 randomized controlled trials with dietary fish, polyphenols, and whole-grain cereals. Am J Clin Nutr. Oct 4 2021;114(4):1342-1350. doi:10.1093/ajcn/nqab188
- Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. European journal of nutrition. 2019;58(1):173-191.
- Kastorini C-M, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. Journal of the American College of Cardiology. 2011;57(11):1299-1313.
- Hamaya R, Ivey KL, Lee DH, et al. Association of diet with circulating trimethylamine-N-oxide concentration. Am J Clin Nutr. Dec 10 2020;112(6):1448-1455. doi:10.1093/ajcn/nqaa225
- Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood Pressure Effects of Sodium Reduction: Dose-Response Meta-Analysis of Experimental Studies. Circulation. Apr 20 2021;143(16):1542-1567. doi:10.1161/circulationaha.120.050371
- Ma Y, He FJ, Sun Q, et al. 24-Hour Urinary Sodium and Potassium Excretion and Cardiovascular Risk. The New England journal of medicine. Jan 20 2022;386(3):252-263. doi:10.1056/NEJMoa2109794
- Neal B, Wu Y, Feng X, et al. Effect of Salt Substitution on Cardiovascular Events and Death. The New England journal of medicine. Sep 16 2021;385(12):1067-1077. doi:10.1056/NEJMoa2105675
- Grandner MA, Fernandez FX. The translational neuroscience of sleep: A contextual framework. Science. Oct 29 2021;374(6567):568-573. doi:10.1126/science.abj8188.
- Lloyd-Jones DM, Allen NB, Anderson CAM, et al. Life's Essential 8: Updating and Enhancing the American Heart Association's Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation. 2022;146(5):e18-e43. doi:doi:10.1161/CIR.0000000000001078. https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000001078
- Liu TZ, Xu C, Rota M, et al. Sleep duration and risk of all-cause mortality: A flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev. Apr 2017;32:28-36. doi:10.1016/j.smrv.2016.02.005.
- Yin J, Jin X, Shan Z, et al. Relationship of Sleep Duration With All-Cause Mortality and Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. J Am Heart Assoc. Sep 9 2017;6(9):e005947. doi:10.1161/JAHA.117.005947. https://www.ncbi.nlm.nih.gov/pubmed/28889101
- He M, Deng X, Zhu Y, Huan L, Niu W. The relationship between sleep duration and all-cause mortality in the older people: an updated and dose-response meta-analysis. BMC Public Health. Jul 28 2020;20(1):1179. doi:10.1186/s12889-020-09275-3.
- Chaput J-P, Dutil C, Featherstone R, et al. Sleep timing, sleep consistency, and health in adults: a systematic review. Applied Physiology, Nutrition, and Metabolism. 2020;45(10 (Suppl. 2)):S232-S247. doi:10.1139/apnm-2020-0032 %M 33054339. https://cdnsciencepub.com/doi/abs/10.1139/apnm-2020-0032
- Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep health . 2015/12/01/ 2015;1(4):233-243. doi:https://doi.org/10.1016/j.sleh.2015.10.004. https://www.sciencedirect.com/science/article/pii/S2352721815001606
- Watson NF, Badr MS, Belenky G, et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. Sleep. Aug 1 2015;38(8):1161-83. doi:10.5665/sleep.4886.
- Blasco-Colmenares E, Moreno-Franco B, Latre ML, et al. Sleep duration and subclinical atherosclerosis: The Aragon Workers' Health Study. Atherosclerosis. 2018/07/01/ 2018;274:35-40. doi:https://doi.org/10.1016/j.atherosclerosis.2018.05.003. https://www.sciencedirect.com/science/article/pii/S0021915018302302
- Yan B, Wu Y, Fan X, Lu Q, Ma X, Bai L. Sleep fragmentation and incidence of congestive heart failure: the Sleep Heart Health Study. Journal of Clinical Sleep Medicine. 2021;17(8):1619-1625. doi:doi:10.5664/jcsm.9270. https://jcsm.aasm.org/doi/abs/10.5664/jcsm.9270 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8656916/pdf/jcsm.9270.pdf
- Huang T, Mariani S, Redline S. Sleep Irregularity and Risk of Cardiovascular Events: The Multi-Ethnic Study of Atherosclerosis. J Am Coll Cardiol. Mar 10 2020;75(9):991-999. doi:10.1016/j.jacc.2019.12.054. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7237955/pdf/nihms-1569277.pdf
- Domínguez F, Fuster V, Fernández-Alvira JM, et al. Association of Sleep Duration and Quality With Subclinical Atherosclerosis. Journal of the American College of Cardiology. 2019;73(2):134-144. doi:10.1016/j.jacc.2018.10.060. https://www.sciencedirect.com/science/article/pii/S0735109718391861?via%3Dihub
- Ooi EL, Rajendran S. Obstructive Sleep Apnea in Coronary Artery Disease. Curr Probl Cardiol. Mar 25 2022:101178. doi:10.1016/j.cpcardiol.2022.101178.
- Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021;144(3):e56-e67. doi:doi:10.1161/CIR.0000000000000988. https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000000988
- Lutsey PL, McClelland RL, Duprez D, et al. Objectively measured sleep characteristics and prevalence of coronary artery calcification: the Multi-Ethnic Study of Atherosclerosis Sleep study. Thorax. Sep 2015;70(9):880-7. doi:10.1136/thoraxjnl-2015-206871. https://thorax.bmj.com/content/thoraxjnl/70/9/880.full.pdf
- CDC. Centers for Disease Control and Prevention. Tips for Better Sleep. Updated 7/15/2016. Accessed 9/7/2022, https://www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
- Chen ML. Sleep Hygiene. In: Berman's Pediatric Decision Making (Fifth Edition). ScienceDirect. https://www.sciencedirect.com/science/article/pii/B9780323054058001285
- AHA. American Heart Association. Sleep plays an important role in heart health. Updated 6/9/2021. Accessed 9/7/2022, https://www.heart.org/en/health-topics/sleep-disorders/sleep-and-heart-health
- Tajik N, Tajik M, Mack I, Enck P. The potential effects of chlorogenic acid, the main phenolic components in coffee, on health: a comprehensive review of the literature. European journal of nutrition. Oct 2017;56(7):2215-2244. doi:10.1007/s00394-017-1379-1. https://link.springer.com/article/10.1007/s00394-017-1379-1
- Chieng D, Canovas R, Segan L, et al. The impact of coffee subtypes on incident cardiovascular disease, arrhythmias, and mortality: long-term outcomes from the UK Biobank. European journal of preventive cardiology. Sep 27 2022;doi:10.1093/eurjpc/zwac189.
- Poole R, Kennedy OJ, Roderick P, Fallowfield JA, Hayes PC, Parkes J. Coffee consumption and health: umbrella review of meta-analyses of multiple health outcomes. BMJ. 2017;359:j5024. doi:10.1136/bmj.j5024. https://www.bmj.com/content/bmj/359/bmj.j5024.full.pdf
- Zheng H, Lin F, Xin N, Yang L, Zhu P. Association of Coffee, Tea, and Caffeine Consumption With All-Cause Risk and Specific Mortality for Cardiovascular Disease Patients. Frontiers in nutrition. 2022;9:842856. doi:10.3389/fnut.2022.842856. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9261910/pdf/fnut-09-842856.pdf
- Xu J, Fan W, Budoff MJ, et al. Intermittent Nonhabitual Coffee Consumption and Risk of Atrial Fibrillation: The Multi-Ethnic Study of Atherosclerosis. J Atr Fibrillation. Jun 2019;12(1):2205. doi:10.4022/jafib.2205. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6811341/pdf/jafib-12-02205.pdf
- Du Y, Lv Y, Zha W, Hong X, Luo Q. Effect of coffee consumption on dyslipidemia: A meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. Nov 27 2020;30(12):2159-2170. doi:10.1016/j.numecd.2020.08.017. https://www.nmcd-journal.com/article/S0939-4753(20)30355-0/fulltext
- Yamagata K. Do Coffee Polyphenols Have a Preventive Action on Metabolic Syndrome Associated Endothelial Dysfunctions? An Assessment of the Current Evidence. Antioxidants (Basel). Feb 4 2018;7(2)doi:10.3390/antiox7020026. https://mdpi-res.com/d_attachment/antioxidants/antioxidants-07-00026/article_deploy/antioxidants-07-00026.pdf?version=1517849221
- Onakpoya IJ, Spencer EA, Thompson MJ, Heneghan CJ. The effect of chlorogenic acid on blood pressure: a systematic review and meta-analysis of randomized clinical trials. J Hum Hypertens. Feb 2015;29(2):77-81. doi:10.1038/jhh.2014.46.
- Lara-Guzmán OJ, Álvarez R, Muñoz-Durango K. Changes in the plasma lipidome of healthy subjects after coffee consumption reveal potential cardiovascular benefits: A randomized controlled trial. Free radical biology & medicine. Nov 20 2021;176:345-355. doi:10.1016/j.freeradbiomed.2021.10.012.
- Higashi Y. Coffee and Endothelial Function: A Coffee Paradox? Nutrients. Sep 4 2019;11(9)doi:10.3390/nu11092104. https://mdpi-res.com/d_attachment/nutrients/nutrients-11-02104/article_deploy/nutrients-11-02104-v2.pdf?version=1568180265
- Azad BJ, Heshmati J, Daneshzad E, Palmowski A. Effects of coffee consumption on arterial stiffness and endothelial function: a systematic review and meta-analysis of randomized clinical trials. Crit Rev Food Sci Nutr. 2021;61(6):1013-1026. doi:10.1080/10408398.2020.1750343.
- Martínez-López S, Sarriá B, Mateos R, Bravo-Clemente L. Moderate consumption of a soluble green/roasted coffee rich in caffeoylquinic acids reduces cardiovascular risk markers: results from a randomized, cross-over, controlled trial in healthy and hypercholesterolemic subjects. European journal of nutrition. Mar 2019;58(2):865-878. doi:10.1007/s00394-018-1726-x. https://link.springer.com/article/10.1007/s00394-018-1726-x
- Ramli NNS, Alkhaldy AA, Mhd Jalil AM. Effects of Caffeinated and Decaffeinated Coffee Consumption on Metabolic Syndrome Parameters: A Systematic Review and Meta-Analysis of Data from Randomised Controlled Trials. Medicina (Kaunas, Lithuania). Sep 11 2021;57(9)doi:10.3390/medicina57090957. https://mdpi-res.com/d_attachment/medicina/medicina-57-00957/article_deploy/medicina-57-00957.pdf?version=1631357228
- Pourmasoumi M, Hadi A, Marx W, Najafgholizadeh A, Kaur S, Sahebkar A. The Effect of Green Coffee Bean Extract on Cardiovascular Risk Factors: A Systematic Review and Meta-analysis. Adv Exp Med Biol. 2021;1328:323-345. doi:10.1007/978-3-030-73234-9_21. https://link.springer.com/chapter/10.1007/978-3-030-73234-9_21
- Ding F, Ma B, Nazary-Vannani A, et al. The effects of green coffee bean extract supplementation on lipid profile in humans: A systematic review and meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. Jan 3 2020;30(1):1-10. doi:10.1016/j.numecd.2019.10.002. https://www.nmcd-journal.com/article/S0939-4753(19)30383-7/pdf
- Asbaghi O, Sadeghian M, Nasiri M, et al. The effects of green coffee extract supplementation on glycemic indices and lipid profile in adults: a systematic review and dose-response meta-analysis of clinical trials. Nutr J. Jul 14 2020;19(1):71. doi:10.1186/s12937-020-00587-z. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7362645/pdf/12937_2020_Article_587.pdf
- Han B, Nazary-Vannani A, Talaei S, et al. The effect of green coffee extract supplementation on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Phytother Res. Nov 2019;33(11):2918-2926. doi:10.1002/ptr.6481. https://onlinelibrary.wiley.com/doi/10.1002/ptr.6481
- Naylor LH, Zimmermann D, Guitard-Uldry M, et al. Acute dose-response effect of coffee-derived chlorogenic acids on the human vasculature in healthy volunteers: a randomized controlled trial. Am J Clin Nutr. Feb 2 2021;113(2):370-379. doi:10.1093/ajcn/nqaa312. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7851825/pdf/nqaa312.pdf
- Suzuki A, Nomura T, Jokura H, Kitamura N, Saiki A, Fujii A. Chlorogenic acid-enriched green coffee bean extract affects arterial stiffness assessed by the cardio-ankle vascular index in healthy men: a pilot study. International journal of food sciences and nutrition. Nov 2019;70(7):901-908. doi:10.1080/09637486.2019.1585763.
- Jiménez-Sánchez A, Martínez-Ortega AJ, Remón-Ruiz PJ, Piñar-Gutiérrez A, Pereira-Cunill JL, García-Luna PP. Therapeutic properties and Use of Extra Virgin Olive Oil in Clinical Nutrition: A Narrative Review and Literature Update. Nutrients. 2022;14(7):1440. https://pubmed.ncbi.nlm.nih.gov/35406067/