Life Extension Magazine®

A genetic defect causes some Americans to have very high cholesterol levels.1
If these high cholesterol levels are not reduced, some victims require coronary artery stents or bypass surgery before age 50.1
We present these data because there has been a debate about the artery-clogging risks posed by LDL cholesterol and its related sub-factors.
The public gets confused when they hear claims that cholesterol plays no role in coronary or cerebral atherosclerosis.
New studies show reductions in cardiovascular deaths and all-cause mortality over the long term when elevated LDL blood levels are reduced.2,3
These recent findings validate the desirability of keeping cholesterol-related blood markers in optimal ranges.
Since the late 1960s people have become more heart-health conscious. This contributed to sharp declines in midlife heart attack and ischemic stroke prevalence.4
Today’s dilemma is that those who escaped arterial blockages in midlife are encountering these issues as they age past 70 years.
We are seeing this in maturing people who have otherwise followed a heart-healthy lifestyle. They sometimes fall victim to occlusive vascular disorders later in life.
One culprit is elevated levels of small dense LDL particles and related blood lipid factors.5,6
This editorial describes safer ways to bring dangerous lipids under control and new data about the risk statin drugs may pose to heart failure patients.
Back in the 1980s, conventional cardiology did not consider LDL cholesterol (LDL) to be a risk factor until blood levels exceeded 159 mg/dL.7
We at Life Extension® argued back then that the optimal LDL level was under 100 mg/dL.
We were challenged by both sides.
Many alternative practitioners did not believe cholesterol was related to occlusive arterial disease, while the conventional crowd stuck to the argument that only people with LDL levels above 159 mg/dL were at highest risk.
The consensus today in most of the conventional world is that LDL blood levels should be below 100 mg/dL in normal aging people and below 70 mg/dL for individuals with higher atherosclerotic cardiovascular disease risk.
Some proactive cardiologists strive to use diet and medication to lower LDL to as little as 30 mg/dL in an attempt to control risk and possibly reverse atherosclerotic disease.
Why the Debate?
It is true, as many have argued, that many heart attacks occur in people with normal cholesterol or LDL cholesterol levels.
This is because cholesterol-related atherogenic risk factors are not the only ones. Multiple other abnormalities increase the risk of atherosclerosis that can lead to a heart attack or stroke.
In other words, arterial blockages can be initiated and promoted by factors other than excess LDL and various related lipid imbalances.
While elevated LDL does not explain all heart attacks and strokes, the role of blood lipids cannot be overlooked.
Low HDL (protective form of cholesterol) combined with elevated LDL, small dense LDL particles, and oxidized LDL all contribute to arterial blockages.
The Statin Drug Dilemma

Statin drugs robustly lower total cholesterol, LDL, and in some trials C-reactive protein. Statins have demonstrated cardiovascular risk-reducing effects in certain specific but large populations.8-10
Statins can cause some people to suffer muscle pain (myalgia) and other side effects when used at the higher doses commonly prescribed.
One of the world’s leading experts on heart failure and CoQ10 has published data on the dangers that statin drugs may present for heart failure patients.
We present info in this month’s issue of Life Extension® suggesting safer ways of lowering excess LDL without inflicting heart damage.
Practical Solutions
Other than in those with a genetic predisposition for very high cholesterol, artery-clogging lipids can be reduced by adhering to strict dietary patterns.
The problem is that few are willing to give up atherogenic foods that include saturated fats (and certain other fats like trans-fat) and high-glycemic starches/sugars.
A practical solution long advocated in this publication, and now supported by a recent clinical trial, indicates that one can achieve desired LDL blood levels by taking a modest statin dose and supplementing with coenzyme Q10.
Lower Dose Statin + CoQ10

A study published in 2019 evaluated participants who suffered from statin-induced muscle pain but needed a statin drug to control LDL cholesterol.
When the statin drug dose was reduced by 50% and CoQ10 supplementation initiated, patients experienced a 29% reduction in pain scores compared to baseline. They also achieved better cholesterol and LDL levels.11
In this study, about 47% of the statin drug users in the CoQ10 group reported a reduction in muscle pain after three months, while only about 7% of statin drug subjects taking placebo (no CoQ10) experienced pain relief.
This study used a less effective form of CoQ10 (ubiquinone) that does not boost CoQ10 blood levels as much as the ubiquinol form of CoQ10, but nonetheless demonstrated remarkable benefits.
CoQ10 Blood Levels
The average baseline CoQ10 blood level in this study (showing reduced statin side effects) was a low 0.759 ug/mL. It increased to 0.875 ug/mL in those supplemented with 100 mg a day of ubiquinone.
Despite the modest 15% boost in CoQ10 blood levels, reductions in statin-induced side effects occurred, along with reduced total cholesterol and LDL in CoQ10-supplemented patients who cut their statin dose in half.
This study shows that reductions in statin drug dose along with CoQ10 therapy can yield similar LDL-lowering benefits and mitigate statin-induced myalgia.11
Not all data indicate that statin drug doses can be cut in half, which is why low-cost blood tests should be utilized to individually manage blood lipid levels.
Studies reported on decades ago in Life Extension® magazine indicate that people should strive for CoQ10 blood levels of around 3.0 ug/mL.12
Those with heart failure should aim to achieve a CoQ10 blood levels of 4.0 ug/mL and higher.13
Statin-Induced Cardiac Toxicity
One innovative cardiologist recently presented data on the impairment of heart muscle function due to statins.14
His hypothesis is based on the depletion of CoQ10 that happens in those taking a statin.
The heart muscle is dependent on CoQ10 to help produce energy, in the form of ATP, to function properly.
Any reduction in energy production can cause cardiac dysfunction.
The authors suggest the existence of a clinical entity designated statin-associated cardiomyopathy and define it as:
“an impairment in heart muscle function secondary to statin drug therapy of a severity sufficient to cause HF [heart failure].”14
Heart failure patients should ask their cardiologists about reducing (or eliminating) statin drug use and increasing their intake of a highly absorbable form of CoQ10 such as ubiquinol.
Landmark Findings on Heart Failure Patients
Peter Langsjoen, MD, is a practicing cardiologist based in Tyler, Texas. He has successfully used high-dose CoQ10 supplements to improve severe heart failure in his patients for decades.14-18
Dr. Langsjoen is a vocal critic of doctors who continue to prescribe statin drugs to heart failure patients without CoQ10 supplementation.
Statin drugs deplete the body’s natural production of coenzyme Q10. This fact is universally accepted.
CoQ10 deficit inflicts horrific effects in cells throughout the body, particularly in the heart, brain and kidneys.11,19-23
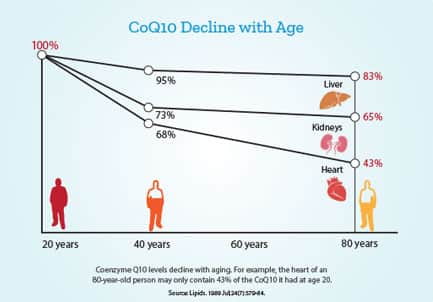
With aging, CoQ10 levels in the body decline.24
Add the CoQ10-depleting impact of statin drugs, and the toxic impact of a CoQ10 deficit can become catastrophic.
Aging and Cardiovascular Disease
Elderly persons suffer epidemic cardiovascular diseases that include:
- Atrial fibrillation
- Aortic valve stenosis
- Slow or rapid heartbeat (bradycardia or tachycardia)
- Coronary artery and capillary occlusion
- Unstable atherosclerotic plaque
- Cerebral artery and capillary blockages
- Chronic heart failure
- Carotid artery stenosis
- Hypercoagulation
- Hypertension
- Vascular inflammation
Despite the frequency of cardio-vascular disorders that occur in older population groups, the risk of heart attack and stroke in the elderly remains under-appreciated and under-treated.
For decades, Life Extension has argued that blood pressure levels have been allowed to remain too high and urged customers to target their blood pressure below 115/75 mmHg.
We fear the same may be true of atherogenic forms of cholesterol. Too many people are still neglecting to optimize their blood lipid levels.
Tell Your Doctor You Do Not Accept “Normal Aging”

Atherosclerosis is a pathological manifestation of aging.
It’s even been observed in ancient mummified bodies. Since people before year 1900 often died under age 50, heart disease was not a leading cause of death as it is today (when lifespans often exceed 80 years in health-conscious individuals).
Adequate protection against heart disease requires blood pressure control along with optimal levels of artery-damaging blood markers such as:
- Homocysteine
- C-reactive protein
- Glucose
- Insulin
- Triglycerides
- Healthy omega ratios
- Cholesterol markers such as: total cholesterol, LDL, small, dense LDL particles, apolipoprotein B, and oxidized LDL.
Most of you make a concerted effort to maintain robust whole-body circulation. This not only reduces mortality risk, but also enhances quality-of-life including heathy cognition.
I hope the data presented in this issue of Life Extension magazine will motivate more readers to optimize ALL cardiovascular risk factors.
In This Month’s Issue…
The article on page 50 describes Dr. Langsjoen’ s research into the dangers of statin drugs in patients with chronic heart failure and how ubiquinol CoQ10 can enable dramatic improvements in these patients.
For those suffering advanced heart failure, the article on page 43 describes an experimental hypo-thesis that involves the removal of senescent cells in the heart. Published data suggest that toxic secretions from senescent cells impede the ability of cardiac progenitor cells to regenerate damaged heart muscles.25
If this concept proves effective, it might remove a biological roadblock that currently prevents cardiac function from being fully restored in heart failure patients.
According to a 2020 report by the American Heart Association one million Americans aged 55 and over are diagnosed with heart failure each year.26
Much of this is preventable in those who maintain healthy coronary artery circulation by keeping vascular risk factors in optimal ranges.
As you will read in this month’s issue, statin drugs are more toxic than most people realize, but so are atherogenic LDL cholesterol particles.
The encouraging news is that one can strike a balance to improve LDL status and reduce statin side effects, if a statin is needed.
The Lab Test Super Sale has been extended to October 5, 2020. To view the many tests included in the Male or Female Panels, please turn to the next page.
To order blood tests call 1-800-208-3444 (24 hours) or log on to: LifeExtension.com/blood
For longer life,
William Faloon
Common Sense Understanding of the Science

For those who question the atherogenic impact of cholesterol, half of men with familial hypercholesterinemia who are untreated will have a heart attack or suffer angina before they turn age 50. Some suffer cardiac disease in their 20s.1
This genetic disorder (familial hyper-cholesterinemia) causes total cholesterol levels to exceed 300 mg/dL.
Men with familial hypercholesterinemia get coronary artery disease 20 years earlier, and women up to 30 years earlier than normal individuals.1
When heart attack prevalence peaked around year 1968, cholesterol levels of around 300 mg/dL were not uncommon.
Those with modestly elevated atherogenic cholesterol factors may prevent their need for coronary artery stents, aortic valve replacement, carotid endarterectomy, bypass surgery, and a host of other hospital treatments.
These conditions will likely develop if preventative steps are not initiated in those with blood lipid imbalances such as low HDL and elevated LDL.
Those seeking healthy longevity, such as readers of Life Extension® magazine, should optimize all known risk factors, including elevated LDL and related atherogenic factors such as excess apolipoprotein B.
References
- Available at: https://www.heart.org/en/health-topics/cholesterol/causes-of-high-cholesterol/familial-hypercholesterolemia-fh. Accessed July 30, 2020.
- Navarese EP, Robinson JG, Kowalewski M, et al. Association Between Baseline LDL-C Level and Total and Cardiovascular Mortality After LDL-C Lowering: A Systematic Review and Meta-analysis. JAMA. 2018 Apr 17;319(15):1566-79.
- Chou R, Dana T, Blazina I, et al. Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016 Nov 15;316(19):2008-24.
- Mensah GA, Wei GS, Sorlie PD, et al. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res. 2017 Jan 20;120(2):366-80.
- Hoogeveen RC, Gaubatz JW, Sun W, et al. Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease: the Atherosclerosis Risk In Communities (ARIC) study. Arterioscler Thromb Vasc Biol.2014 May;34(5):1069-77.
- Gidding SS, Allen NB. Cholesterol and Atherosclerotic Cardiovascular Disease: A Lifelong Problem. J Am Heart Assoc.2019 Jun 4;8(11):e012924.
- Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. The Expert Panel. Arch Intern Med. 1988 Jan;148(1):36-69.
- Available at: https://www.uptodate.com/contents/management-of-elevated-low-density-lipoprotein-cholesterol-ldl-c-in-primary-prevention-of-cardiovascular-disease. Accessed July 29, 2020.
- Available at: https://www.uptodate.com/contents/management-of-low-density-lipoprotein-cholesterol-ldl-c-in-the-secondary-prevention-of-cardiovascular-disease. Accessed July 29, 2020.
- Asher J, Houston M. Statins and C-reactive protein levels. J Clin Hypertens (Greenwich). 2007 Aug;9(8):622-8.
- Derosa G, D’Angelo A, Maffioli P. Coenzyme q10 liquid supplementation in dyslipidemic subjects with statin-related clinical symptoms: a double-blind, randomized, placebo-controlled study. Drug Des Devel Ther. 2019;13:3647-55.
- Available at: https://www.lifeextension.com/magazine/2008/2/conventional-coq10-fails-severe-heart-disease-patients. Accessed July 29, 2020.
- Langsjoen PH, Langsjoen AM. Supplemental ubiquinol in patients with advanced congestive heart failure. Biofactors. 2008;32(1-4):119-28.
- Langsjoen PH, Langsjoen JO, Langsjoen AM, et al. Statin-Associated Cardiomyopathy Responds to Statin Withdrawal and Administration of Coenzyme Q10. Perm J. 2019;23:18-257.
- Langsjoen PH, Langsjoen A, Willis R, et al. Treatment of hypertrophic cardiomyopathy with coenzyme Q10. Mol Aspects Med. 1997;18 Suppl:S145-51.
- Langsjoen PH, Langsjoen PH, Folkers K. A six-year clinical study of therapy of cardiomyopathy with coenzyme Q10. Int J Tissue React. 1990;12(3):169-71.
- Langsjoen PH, Langsjoen PH, Folkers K. Isolated diastolic dysfunction of the myocardium and its response to CoQ10 treatment. Clin Investig. 1993;71(8 Suppl):S140-4.
- Langsjoen PH, Folkers K, Lyson K, et al. Pronounced increase of survival of patients with cardiomyopathy when treated with coenzyme Q10 and conventional therapy. Int J Tissue React. 1990;12(3):163-8.
- Molyneux SL, Florkowski CM, George PM, et al. Coenzyme Q10: an independent predictor of mortality in chronic heart failure. J Am Coll Cardiol. 2008 Oct 28;52(18):1435-41.
- Kumar A, Kaur H, Devi P, et al. Role of coenzyme Q10 (CoQ10) in cardiac disease, hypertension and Meniere-like syndrome. Pharmacol Ther. 2009 Dec;124(3):259-68.
- Kim J, Medsinge A, Chauhan B, et al. Coenzyme Q10 in the Treatment of Corneal Edema in Kearns-Sayre: Is There an Application in Fuchs Endothelial Corneal Dystrophy? Cornea. 2016 Sep;35(9):1250-4.
- Mancuso M, Orsucci D, Calsolaro V, et al. Coenzyme Q10 and Neurological Diseases. Pharmaceuticals (Basel). 2009 Dec 1;2(3):134-49.
- Mantle D, Hargreaves I. Coenzyme Q10 and Degenerative Disorders Affecting Longevity: An Overview. Antioxidants (Basel). 2019 Feb 16;8(2):44.
- Kalen A, Appelkvist EL, Dallner G. Age-related changes in the lipid compositions of rat and human tissues. Lipids. 1989 Jul;24(7):579-84.
- Lewis-McDougall FC, Ruchaya PJ, Domenjo-Vila E, et al. Aged-senescent cells contribute to impaired heart regeneration. Aging Cell. 2019 Jun;18(3):e12931.
- Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020 Mar 3;141(9):e139-e596.

