Life Extension Magazine®

Healthy arteries expand and contract smoothly with each heartbeat.
With age, soft tissues such as arteries stiffen and lose youthful flexibility.
The phrase “hardening of the arteries” describes loss of arterial elasticity and obstructed blood flow. This “hardening” is an important predictor of heart attack and stroke.1-3
In severe cases, the aortic artery becomes so stiff and brittle that it cannot be repaired.
This is how actress Lucille Ball died. She suffered a dissecting aortic aneurysm that surgeons spent many hours repairing. They replaced her aortic valve and five inches of her upper aortic artery. It was too risky to attempt to replace her entire aortic artery. One week later Lucy died from a second rupture in her lower (abdominal) aorta.4
Lucy, with her incredible fame and fortune, perished from the structural failure of the largest artery (the aorta) in her body.
Arterial stiffness is associated with increased risk of cardiovascular disorders, dementia, and death.5-11 When the aorta stiffens, it elevates blood pressure as the heart must pump harder to force blood through the body.
Factors that contribute to arterial stiffness include inflammation, glycation, hypertension, and poor glucose control.12-15
A less understood cause of arterial stiffening is calcification.16
In 1999, we published a report on the importance of consuming high-dose vitamin K to block calcium infiltration into our soft tissues.17
Over the years we received many calls asking if higher dose vitamin K2 could reverse vascular calcification. Until recently, we did not know the answer.
In 2007, an animal study demonstrated significant reduction of arterial calcification in response to vitamin K supplementation.18 While intriguing, we did not know if this would work in people.
A landmark clinical trial using a long-acting form of vitamin K2 has demonstrated significant reductions of arterial stiffening in humans.19
This provides us all with an opportunity to restore more youthful flexibility to aging blood vessels and other soft tissues.
Modern medicine combined with healthier lifestyles has enabled maturing people to postpone the time when they suffer vascular-related disorders.
Protection against coronary artery occlusion can be achieved in mid-life via control of lipids, glucose, and pro-inflammatory factors.20-24
As people age past 65 years, however, the cumulative buildup of soft-tissue calcification sharply elevates incidence of stroke, heart failure and aortic valve stenosis.1,2,25-28
Heart Valve Disorders

Each year more than five million Americans are diagnosed with heart valve disorders.29
Without treatment, about 50% of those with symptomatic aortic stenosis will die within two years.30
While drugs known as ACE inhibitors (angiotensin-converting enzyme inhibitors) may slow progression of early-stage aortic valve stenosis, surgical interventions are the only way to treat advanced aortic stenosis.31,32
People with surgically-replaced aortic valves often require lifelong anticoagulant drugs to reduce ischemic stroke risk.33
A more rational approach to reduce the epidemic of vascular disorders facing the elderly is to block soft-tissue calcification starting earlier in life. This is readily accomplished with low-cost vitamin K2 supplements.
While it’s never too late to impede soft-tissue calcification, the dilemma facing aging humans is how to reverse arterial stiffness that occurred before the importance of taking vitamin K was recognized.
Aortic Valve Calcification and Aortic Stenosis
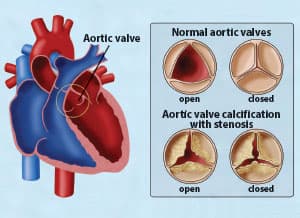 |
A healthy aortic valve opens and closes normally. However, calcification of the aortic valve, also called aortic sclerosis, frequently occurs with advancing age. In the United States, this age-related calcification of the aortic valve is the number one cause of aortic stenosis, which is a narrowing of the valvular outflow tract. Over time, the heart muscle weakens as a result of aortic stenosis, and can progress to heart failure.
Preventable Causes of Aortic Valve Calcification and Aortic Stenosis
Aging is considered a risk factor for aortic valve calcification and aortic stenosis. Congenital defects and infections can also severely damage the aortic valve.31,32,34
A large case-control study showed that the calcific degeneration observed in severe aortic stenosis is increased by these unhealthy factors:35
| Hypertension | 117% |
| History of smoking | 72% |
| Cholesterol (>200 mg/dL) | 111% |
| Obesity | 103% |
Gaining control over these risk factors for aortic valve stenosis can enable aging people to dramatically reduce their overall mortality risk.
Measuring Arterial Health
Calcification inflicts severe injury to arteries and heart valves.36-38 The pictures on this page show deformed calcified aortic valves.
Observational studies show lower prevalence of coronary disease and arterial calcification in those with higher intake of vitamin K2.39-42
The “gold standard” for measuring regional arterial stiffness is the “carotid-femoral pulse wave velocity” test.43,44
People who score poorly on this test have higher rates of cardiovascular diseases.
Reversing Arterial Stiffness
A clinical trial was designed using carotid-femoral pulse wave velocity as one of the tests to evaluate the effects of supplementing with 180 mcg a day of a long-acting form of vitamin K2 (MK-7).19
This randomized, placebo-controlled study was comprised of 244 postmenopausal women aged 55-65 years. Baseline tests of arterial stiffness were performed and the tests repeated yearly for three years.
At the end of three years, otherwise healthy postmenopausal women in the vitamin K2 group experienced a statistically significant 5.8% reduction in the stiffness index beta, a parameter for arterial stiffness, and a 3.6% reduction in carotid-femoral pulse wave velocity. The placebo group had a slight increase of 1.3% in the stiffness index and a 0.22% increase in carotid-femoral pulse wave velocity.19
The benefit was conferred upon the women with a higher baseline index of arterial stiffness in comparison with those women with lower baseline levels of arterial stiffness. This suggests that those postmenopausal women with more advanced atherosclerosis derive more benefit with vitamin K2.
This is the first long-term human trial showing improvements in measures of arterial stiffness in response to long-acting vitamin K2. While the 5.8% and 3.6% improvements might not appear substantial, when realizing that calcification often worsens with age, the fact that there was a reversal in arterial stiffness compared to placebo is quite remarkable.
This study helps support population-based studies associating higher intake of vitamin K2 with reduced cardiovascular incidence and mortality.39,42,45
Importance of Calcium Balance

Calcium is essential to sustain life.
Without sufficient calcium, we would not be able to maintain the electrolyte balance needed for proper rhythmic heart beats.46 If one were to deplete their bloodstream of calcium, they would die from a heart attack caused by an acute arrhythmic disorder.47
In a healthy body, 99% of calcium is stored in bone where it provides structural support.48 The amount of calcium allowed into the bloodstream is tightly controlled.49
In our bones, vitamin K2 activates proteins that beneficially bind calcium to bone.50 Human populations with high dietary intake of vitamin K2 have lower rates of osteoporosis.51-56
How K2 Prevents Vascular Calcification
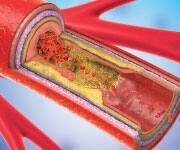
coronary artery.
Vitamin K activates your body’s ability to store calcium in the bone (where it belongs) and blocks it from infiltrating soft tissues.42,45,56
To visualize how vitamin K2 protects against calcification, just imagine a protein lining your vascular system that allows calcium in or out. The factor that regulates whether this protein is turned “on”—meaning it blocks calcium infiltration—is vitamin K2.
Vitamin K2 activates matrix GLA proteins in soft tissues to keep calcium out.40,42 On the flip side, K2 activates calcium-binding proteins in bone to maintain skeletal density.50
In the absence of vitamin K, bony structures form in soft tissues. Early pathologists discovered that arteries that are soft and pliable in youth often turned to stone in the elderly.57
Modern findings demonstrate the power of vitamin K, or lack thereof, to control whether we maintain strong bone density and soft pliable tissues, or develop osteoporosis together with vascular calcification.
The take home lesson as it relates to healthy blood flow is:
Matrix GLA Protein + Vitamin K2 = Barrier against calcium infiltration
Matrix GLA Protein – Vitamin K2 = Vascular/soft tissue calcification
Where We Stand Today
Most adults probably suffer some degree of calcification, as intake of vitamin K2 in Western societies remains at low levels.
A study published in 2007 tested vitamin K1 and the MK-4 form of vitamin K2 on rats.18
In the groups receiving high-dose vitamin K1 or K2 (MK-4), not only was there no further arterial calcium accumulation, there was a 37% reduction of previously accumulated arterial calcification after six weeks. After 12 weeks, there was a 53% reduction in accumulated arterial calcium deposits.
The groups receiving the high-dose vitamin K1 and K2 also showed a reversal in carotid artery stiffness. This study provided intriguing evidence that vascular calcification may be reversible by high vitamin K intake.18
When we reported on this study, we postulated that people taking vitamin K supplements over an extended time period “might” induce a regression of arterial calcification. We emphasized, however, that “more human research is needed to establish this.”
That human research has now demonstrated (for the first time) a significant improvement in arterial health in postmenopausal women with higher arterial stiffness who supplement with a modest dose of vitamin K2.19
This study also demonstrated a favorable 50% decrease in a marker of a calcium-blocking protein in the K2 supplemented group compared to placebo.19 Previous studies show that people with higher levels of this circulatory marker (uncarboxylated matrix GLA protein) have elevated rates of chronic kidney disease and heart failure.58-60
For those who like technical details, vitamin K2 is essential for the enzyme that “carboxylates” the matrix GLA protein. When matrix GLA is “carboxylated,” it shields arteries from calcium infiltration. Uncarboxylated matrix GLA, on the other hand, facilitates vascular calcification.58-60
In the new human study described in this article, a modest dose of vitamin K2 reduced uncarboxylated matrix GLA by 50%, which is an indicator of improved cardiovascular health.19
What are Ideal Vitamin K Supplements?

A review of the published scientific literature provides a rationale for aging people to supplement with three different forms of vitamin K. These include vitamin K1, vitamin K2 (MK-4), and vitamin K2 (MK-7).40,45,61
Since vitamin K is fat-soluble, taking it with the fattiest meal of the day will augment absorption into one’s bloodstream.
Some may ask why not take just the MK-7 form of vitamin K2 since this has long-acting effects in the body and has demonstrated powerful calcium-blocking properties.
Our response is that vitamin K1 and MK-4 have demonstrated impressive results in other studies, so it is best to take a formula that contains all three forms of vitamin K.
Interestingly, the MK-4 form of vitamin K2 has been used in very high doses as a prescription drug in Japan to treat osteoporosis.62
Since vitamin K1 and MK-4 are inexpensive, it makes sense to include them with long-acting MK-7 vitamin K2 to inhibit and possibly reverse as much vascular calcification as possible, while providing support for strong bones.
Potential to Spare Millions of Lives
An enormous body of published evidence indicates that common degenerative illnesses striking aging humans may be prevented by taking sufficient potencies of the proper forms of vitamin K.
Yet most physicians don’t understand vitamin K’s critical role of blocking calcification of heart valves, arterial linings, and other soft tissues, while keeping calcium in bone where it is needed.
Eye-opening studies shed light on the importance for people of all ages to optimize their intake of vitamin K to protect against soft tissue calcification.
An urgent need exists to convey this information to the medical community. This may not happen any time soon because vitamin K is sold as a low-cost dietary supplement and not an expensive prescription drug.
For longer life,
William Faloon, Co-Founder
Life Extension Buyers Club
References
- Leening MJ, Elias-Smale SE, Kavousi M, et al. Coronary calcification and the risk of heart failure in the elderly: the Rotterdam Study. JACC Cardiovasc Imaging. 2012;5(9):874-80.
- Hermann DM, Gronewold J, Lehmann N, et al. Coronary artery calcification is an independent stroke predictor in the general population. Stroke. 2013;44(4):1008-13.
- Vliegenthart R, Hollander M, Breteler MM, et al. Stroke is associated with coronary calcification as detected by electron-beam CT: the Rotterdam Coronary Calcification Study. Stroke. 2002;33(2):462-5.
- Available at: http://articles.latimes.com/1989-04-27/news/mn-1629_1_aorta-blood-vessel-aortic. Accessed August 2, 2017.
- Mattace-Raso FU, van der Cammen TJ, Hofman A, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113(5):657-63.
- Cecelja M, Chowienczyk P. Role of arterial stiffness in cardiovascular disease. JRSM Cardiovasc Dis. 2012;1(4).
- Mitchell GF, Hwang SJ, Vasan RS, et al. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation. 2010;121(4):505-11.
- Pase MP, Herbert A, Grima NA, et al. Arterial stiffness as a cause of cognitive decline and dementia: a systematic review and meta-analysis. Intern Med J. 2012;42(7):808-15.
- Rabkin SW. Arterial stiffness: detection and consequences in cognitive impairment and dementia of the elderly. J Alzheimers Dis. 2012;32(3):541-9.
- Watson NL, Sutton-Tyrrell K, Rosano C, et al. Arterial stiffness and cognitive decline in well-functioning older adults. J Gerontol A Biol Sci Med Sci. 2011;66(12):1336-42.
- Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55(13):1318-27.
- Park S, Lakatta EG. Role of inflammation in the pathogenesis of arterial stiffness. Yonsei Med J. 2012;53(2):258-61.
- Dweck MR, Jones C, Joshi NV, et al. Assessment of valvular calcification and inflammation by positron emission tomography in patients with aortic stenosis. Circulation. 2012;125(1):76-86.
- McNulty M, Mahmud A, Feely J. Advanced glycation end-products and arterial stiffness in hypertension. Am J Hypertens. 2007;20(3):242-7.
- Elewa U, Fernandez-Fernandez B, Alegre R, et al. Modifiable risk factors for increased arterial stiffness in outpatient nephrology. PLoS One. 2015;10(4):e0123903.
- Mackey RH, Venkitachalam L, Sutton-Tyrrell K. Calcifications, arterial stiffness and atherosclerosis. Adv Cardiol. 2007;44:234-44.
- Available at: http://www.lifeextension.com/magazine/2000/2/report/page-01. Accessed August 11, 2017.
- Schurgers LJ, Spronk HM, Soute BA, et al. Regression of warfarin-induced medial elastocalcinosis by high intake of vitamin K in rats. Blood. 2007;109(7): 2823-31.
- Knapen MH, Braam LA, Drummen NE, et al. Menaquinone-7 supplementation improves arterial stiffness in healthy postmenopausal women. A double-blind randomised clinical trial. Thromb Haemost. 2015;113(5):1135-44.
- Pletcher MJ, Bibbins-Domingo K, Liu K, et al. Nonoptimal lipids commonly present in young adults and coronary calcium later in life: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Ann Intern Med. 2010;153(3): 137-46.
- Yam D, Bott-Kanner G, Genin I, et al. The effect of omega-3 fatty acids on risk factors for cardiovascular diseases. Harefuah. 2001;140(12):1156-8, 230.
- Li Q, Chen AH, Song XD, et al. Analysis of glucose levels and the risk for coronary heart disease in elderly patients in Guangzhou Haizhu district. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30(6):1275-8.
- Koenig W, Sund M, Frohlich M, et al. C-Reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99(2):237-42.
- Ridker PM, Rifai N, Stampfer MJ, et al. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000;101(15):1767-72.
- Rothwell PM, Gibson R, Warlow CP. Interrelation between plaque surface morphology and degree of stenosis on carotid angiograms and the risk of ischemic stroke in patients with symptomatic carotid stenosis. On behalf of the European Carotid Surgery Trialists’ Collaborative Group. Stroke. 2000;31(3):615-21.
- Faggiano P, Antonini-Canterin F, Baldessin F, et al. Epidemiology and cardiovascular risk factors of aortic stenosis. Cardiovasc Ultrasound. 2006;4:27.
- Lindman BR, Bonow RO, Otto CM. Current management of calcific aortic stenosis. Circ Res. 2013;113(2):223-37.
- Ramaraj R, Sorrell VL. Degenerative aortic stenosis. Bmj. 2008;336(7643):550-5.
- Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368(9540):1005-11.
- Otto CM, Prendergast B. Aortic-valve stenosis--from patients at risk to severe valve obstruction. N Engl J Med. 2014;371(8):744-56.
- Liakos CI, Grassos CA, Papadopoulos DP, et al. Arterial hypertension and aortic valve stenosis: Shedding light on a common “liaison”. Hellenic J Cardiol. 2017.
- Rajamannan NM. Is it time for medical therapy for aortic valve disease? Expert Rev Cardiovasc Ther. 2004;2(6):845-54.
- Available at: https://www.ncbi.nlm.nih.gov/books/NBK47039/. Accessed August 11, 2017.
- Lindroos M, Kupari M, Valvanne J, et al. Factors associated with calcific aortic valve degeneration in the elderly. Eur Heart J. 1994;15(7):865-70.
- Peltier M, Trojette F, Sarano ME, et al. Relation between cardiovascular risk factors and nonrheumatic severe calcific aortic stenosis among patients with a three-cuspid aortic valve. Am J Cardiol. 2003;91(1):97-9.
- Wayhs R, Zelinger A, Raggi P. High coronary artery calcium scores pose an extremely elevated risk for hard events. J Am Coll Cardiol. 2002;39(2):225-30.
- Sangiorgi G, Rumberger JA, Severson A, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998;31(1):126-33.
- Vliegenthart R, Oudkerk M, Hofman A, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation. 2005;112(4):572-7.
- Geleijnse JM, Vermeer C, Grobbee DE, et al. Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam Study. J Nutr. 2004;134(11):3100-5.
- Gast GC, de Roos NM, Sluijs I, et al. A high menaquinone intake reduces the incidence of coronary heart disease. Nutr Metab Cardiovasc Dis. 2009;19(7):504-10.
- Beulens JW, Bots ML, Atsma F, et al. High dietary menaquinone intake is associated with reduced coronary calcification. Atherosclerosis. 2009;203(2):489-93.
- Shea MK, Holden RM. Vitamin K status and vascular calcification: evidence from observational and clinical studies. Adv Nutr. 2012;3(2):158-65.
- Kubozono T, Ohishi M. Prognostic Significance of Regional Arterial Stiffness for Stroke in Hypertension. Pulse (Basel). 2015;3(2):98-105.
- Covic A, Siriopol D. Pulse wave velocity ratio: the new “gold standard” for measuring arterial stiffness. Hypertension. 2015;65(2):289-90.
- Maresz K. Proper Calcium Use: Vitamin K2 as a Promoter of Bone and Cardiovascular Health. Integr Med (Encinitas). 2015;14(1):34-9.
- Soar J, Perkins GD, Abbas G, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 2010;81(10):1400-33.
- Available at: https://medlineplus.gov/cardiacarrest.html. Accessed August 21, 2017.
- Bonjour JP. Calcium and phosphate: a duet of ions playing for bone health. J Am Coll Nutr. 2011;30(5 Suppl 1):438s-48s.
- Available at: http://www.parathyroid.com/parathyroid-function.htm. Accessed August 14, 2017.
- Hauschka PV. Osteocalcin: the vitamin K-dependent Ca2+-binding protein of bone matrix. Haemostasis. 1986;16(3-4):258-72.
- Tsukamoto Y. Studies on action of menaquinone-7 in regulation of bone metabolism and its preventive role of osteoporosis. Biofactors. 2004;22(1-4): 5-19.
- Plaza SM, Lamson DW. Vitamin K2 in bone metabolism and osteoporosis. Altern Med Rev. 2005;10(1):24-35.
- Yamaguchi M. Regulatory mechanism of food factors in bone metabolism and prevention of osteoporosis. Yakugaku Zasshi. 2006;126(11):1117-37.
- Fujita Y, Iki M, Tamaki J, et al. Association between vitamin K intake from fermented soybeans, natto, and bone mineral density in elderly Japanese men: the Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) study. Osteoporos Int. 2012;23(2):705-14.
- Bullo M, Estruch R, Salas-Salvado J. Dietary vitamin K intake is associated with bone quantitative ultrasound measurements but not with bone peripheral biochemical markers in elderly men and women. Bone. 2011;48(6):1313-8.
- Jie KG, Bots ML, Vermeer C, et al. Vitamin K status and bone mass in women with and without aortic atherosclerosis: a population-based study. Calcif Tissue Int. 1996;59(5):352-6.
- Virchow R. Cellular pathology as based upon physiological and pathological histology. Philadelphia: J.B. Lippincott and Co.; 1863.
- Cranenburg EC, Vermeer C, Koos R, et al. The circulating inactive form of matrix Gla Protein (ucMGP) as a biomarker for cardiovascular calcification. J Vasc Res. 2008;45(5):427-36.
- Schurgers LJ, Cranenburg EC, Vermeer C. Matrix Gla-protein: the calcification inhibitor in need of vitamin K. Thromb Haemost. 2008;100(4):593-603.
- Theuwissen E, Smit E, Vermeer C. The role of vitamin K in soft-tissue calcification. Adv Nutr. 2012;3(2):166-73.
- Komai M, Shirakawa H. [Vitamin K metabolism. Menaquinone-4 (MK-4) formation from ingested VK analogues and its potent relation to bone function]. Clin Calcium. 2007;17(11):1663-72.
- Tanaka S, Miyazaki T, Uemura Y, et al. Design of a randomized clinical trial of concurrent treatment with vitamin K2 and risedronate compared to risedronate alone in osteoporotic patients: Japanese Osteoporosis Intervention Trial-03 (JOINT-03). J Bone Miner Metab. 2014;32(3):298-304.

