Life Extension Magazine®
The most dangerous time of the day is often right after you eat.
That’s when insulin and glucose flood your bloodstream during the digestion of your meal.
Even if you are not diabetic, this tidal wave of after-meal insulin and glucose can cause lasting damage that leads to increased risk of stroke, heart attack, dementia, and diabetes.1-3
Life Extension® has expended tremendous effort over the years seeking practical methods to reduce the impact of the glucose/insulin spikes that follow most meals.
Scientists have identified two unique plant extracts, maqui-berry and clove extract, that markedly mitigate after-meal surges in blood glucose and insulin levels.
In a human trial, researchers found that standardized maqui-berry extract delayed and lowered dangerous after-meal glucose levels and reduced after-meal insulin spikes (by a startling 56% compared to the placebo group).4
In another human trial, clove flower dropped after-meal glucose levels to about the same as the before-meal values.5
The discovery of natural compounds that can safely reduce the impact of after-meal increases in glucose and insulin blood levels has significant public health implications.
After-Meal Glucose and Insulin Accelerate Aging
Glucose and insulin in the bloodstream can rapidly climb after any meal, especially a large meal with concentrated carbohydrates.
This after-meal surge in glucose and insulin spreads throughout the body several hours following a meal.
That means for several hours each day, our tissues are soaked in a high-glucose/high-insulin environment. During the critical two-hour period following a meal, most experts agree that maximum damage can occur due to the surge in glucose and insulin.6
Even if you are not diabetic, these after-meal surges in glucose and insulin create damage. Over time, this leads to a downward spiral that harms every organ in the body and accelerates aging processes.
In fact, glucose levels during the after-meal period are typically so high that glucose chemically bonds to proteins and fats throughout the body. This process is called glycation.
To reduce glycation-induced aging, we need to find ways to minimize our exposure to excessive blood glucose and insulin.
Elevated After-Meal Glucose and Insulin Wreaks Systemic Havoc
When insulin and glucose rapidly surge following high carbohydrate meals, tissues and cells within the body can be damaged.
One result is initiation of inflammatory responses that create metabolic havoc.1,7-9
This may be viewed as one giant, destructive insult that occurs after almost every meal.
These acute changes, which may not be immediately noticeable, do add up over a lifetime. The result is accelerated aging that can hasten the conditions that lead to premature death.
While this phenomenon is most obvious in people who are true diabetics, every human suffers from damage caused by abnormal postprandial (after-meal) metabolism. A brief list of this constant damage inflicted by abnormal postprandial metabolism:
- Cloudiness of the lens with cataracts
- Degeneration of retinas, which leads to potential blindness
- Decline in brain function that opens the door to dementia, including Alzheimer’s disease
- Decline in kidney function, leading to renal failure
- Stiffening of heart muscle and arteries, creating the opportunity for stroke, heart attacks and heart failure – all processes that, given enough time, will occur in any of us
In fact, elevated blood glucose concentrations following a meal are highly predictive of future disease risks, even in people whose fasting blood glucose levels are normal.1,10
Maqui-Berry Extract Slows Glucose Absorption
Maqui berries have demonstrated many health benefits.
In a new discovery, maqui-berry extract has been shown to lower after-meal rises in both glucose and insulin.
Research suggests that a standardized extract of maqui berries contains compounds known as delphinidins.
These fruit-based compounds stimulate a peptide that lowers postprandial (after-meal) blood glucose and can have a moderating influence on insulin spikes.11
The name of this peptide naturally secreted by the body is glucagon-like peptide-1 (GLP-1).
In the stomach, GLP-1 has the effect of slowing and delaying emptying. This means that glucose from the meal reaches the absorptive tissue in the small intestine later, and in lower quantities, than it would otherwise do. GLP-1 thus helps limit after-meal glucose spikes.12,13
Maqui-berry extract has also been shown to slow the rise of after-meal insulin levels.4
FIGURE 1: Standardized Maqui-Berry Extract Inhibits Postprandial Glucose and Insulin Elevations
 |
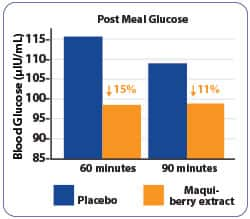 |
Standardized maqui-berry extract inhibits postprandial rises in plasma glucose and decreases postprandial insulin.4 Levels of postprandial glucose (right) and insulin (left), show the percentage decrease in these parameters by standardized maqui-berry extract treatment (orange) as compared to placebo (blue).
Damaging Effects of Excess Insulin
Insulin is a crucial hormone for the metabolism of carbohydrates, fats, and proteins. In a perfect scenario, after ingestion of foods, insulin is released in moderated amounts to help shuttle glucose into the cells for energy production or storage and then should drop back to pre-meal levels.14,15
But for many individuals this is not the case, and the decreased ability of the body’s cells to respond to insulin creates a condition known as insulin resistance.
As a result, the pancreas produces more insulin than normal, creating a state of hyperinsulinemia that sets the path for multiple age-related diseases, like atherosclerosis, hypertension, lipid abnormalities, chronic inflammation, type II diabetes, obesity, and cancer.16-27
Once insulin levels begin to rise, it is difficult to control and can lead to multiple degenerative disorders.
Over time, the body becomes insulin resistant and needs more and more insulin to process a normal meal.
Excess insulin is one of the quickest routes to accelerated aging, thus making insulin control a key factor in any longevity program. This is where the benefits of maqui berry are of key importance.
What You Need to Know
 |
Control Postprandial Blood-Glucose Levels
- While glucose is an absolute necessity to fuel human life, if elevated, it poses a long-term threat to the integrity of our tissues, organs, and systems.
- Postprandial (after-meal) elevations in blood glucose and insulin are increasingly recognized as major threats to metabolic health.
- Both type II diabetes and cardiovascular disease risks are sharply elevated in people whose postprandial glucose levels are high, but physicians rarely bother to measure postprandial glucose, and even fewer still measure after-meal insulin.
- Most physicians, at present, will not prescribe prescription drugs until diabetes is fully-developed—long after the window of opportunity for prevention has closed.
- But control of postprandial glucose and insulin is indeed possible, with the introduction of standardized maqui-berry and water-soluble clove extracts.
- These natural compounds work by complementary mechanisms to suppress after-meal metabolic derangements, thereby reducing the risk of tissue and cellular damage.
Maqui Berry Reduces Glucose and Insulin Spikes

In a promising study, subjects taking a standardized maqui-berry extract experienced both a lower postprandial blood glucose level and a 56% lower insulin spike at 60 minutes.4
For the study, ten volunteers were enrolled who had fasting glucose levels less than 100 mg/dL (which is considered normal). They were given a standard white rice meal and their blood glucose levels two-hours after were at least 100 mg/dL but less than 125 mg/dL. This is considered “altered glucose tolerance,” but nowhere near as bad as diabetics whose two-hour after-meal glucose can approach 190 mg/dL.4
Subjects in this study were then given either 200 mg of standardized maqui-berry extract or a similar-looking placebo.
Thirty minutes after ingestion of the maqui-berry extract or placebo, all subjects received a small meal of 75 grams (about 2.5 ounces) of white rice, calculated to produce a significant rise in postprandial glucose levels.
Blood was drawn before (baseline) and at 15, 30, 60, 90, 120, and 180 minutes after the rice meal for measurements of glucose concentrations.
Results showed that the single dose of 200 mg of standardized maqui-berry extract decreased both postprandial glucose and insulin levels compared with those subjects taking the placebo.
Placebo recipients showed a peak postprandial glucose level of approximately 115 mg/dL at one hour, which had fallen to about 110 mg/dL by 90 minutes.
Subjects receiving the standardized maqui-berry extract did not experience peak glucose concentrations until two hours after the meal and the level was only about 107 mg/dL. This means that the maqui-berry extract was able to safely slow down the rise in post meal glucose.
Prior to these two hours, the maqui-berry group’s glucose levels rose only to around 98 mg/dL at 60 and 90 minutes.
In placebo subjects, insulin concentrations steadily rose to peak (average of 25.33 µIU/ml) at 60 minutes. However, in the maqui-berry group, insulin levels rose much more slowly, on average to 11.22 µIU/ml at 60 minutes. This is 56% lower than in the placebo group.
In addition, insulin level peak in the maqui-berry group was delayed much longer, until 90 minutes. More importantly, the insulin levels for the standardized maqui-berry-extract group peaked at a much lower level than that of the placebo group.4
This is of extreme importance, because research increasingly shows that insulin, in excess, may be a contributor to a variety of age-related disorders, including some types of cancer.28
Glucose Increases Cancer Mortality
The link between diabetes and increased cancer risk is well established but often overlooked by mainstream medicine. In an alarming 2017 review of the literature, researchers showed that cancer mortality increased in prediabetic individuals.35
For the review, the team of researchers evaluated studies between 1966 and 2016 that looked at cancer mortality at the nondiabetic levels (defined as fasting plasma glucose of <126 mg/dL and a two-hour plasma glucose of <200 mg/dL after oral glucose tolerance test).
From the seven studies identified, men with elevated fasting glucose levels had an increase in cancer mortality. Individuals with impaired glucose tolerance (prediabetic) after oral glucose tolerance tests were also at an increase for cancer mortality. For cause-cancer mortality in prediabetics, an increase mortality was seen for stomach, liver, and pancreatic cancers.
The role of elevated glucose levels as an indicator of cancer mortality is evident. The studies discussed in this article provide evidence of two natural extracts that can help control two of the deadliest players in age related diseases, glucose and insulin.
Maqui Berry Lowers HbA1c Levels

In a separate study, standardized maqui-berry extract showed promise in reducing hemoglobin A1c (HbA1c).
The study was done on people who were newly-identified as “prediabetic.” They had either “mildly” elevated fasting blood glucose (greater than 100 mg/dL up to 125 mg/dL), or immediate postprandial glucose of more than 140 mg/dL or two-hour postprandial glucose of greater than 120 mg/dL.29
After researchers measured and established baseline levels of HbA1c in the patient group, all of the subjects were given 180 mg of standardized maqui-berry extract. They were then instructed to take the standardized maqui-berry extract each morning for 90 days and to avoid eating large food portions (especially carbohydrates) on days prior to their follow-ups at the clinic, which lasted 90 days. Then the researchers followed up with measuring HbA1c levels at 30, 60, and 90 days from the start.29
Hemoglobin A1c levels declined at 60 days, and by 90 days, this marker of long term glucose control (HbA1c) was down by 0.3% from 5.65% to 5.35% (See Figure 2).29
FIGURE 2: Standardized Maqui-Berry Extract Lowers Glycated Hemoglobin Levels
 |
Standardized maqui-berry extract treatment in subjects with prediabetes decreases glycated hemoglobin.29 Hemoglobin A1c was measured in subjects consuming 180 mg standardized maqui-berry extract daily for 90 days. A1c levels declined 0.3% after 90 days of maqui-berry supplementation.
Clove Extract Prevents Postprandial Glucose Spikes

Searching for natural compounds that can be used to control after-meal blood glucose, researchers also began investigating a water-soluble extract of the clove flower bud (Syzygium aromaticum).
An analysis of a water-soluble clove extract found that it contains polyphenols capable of regulating the enzyme responsible for freeing glucose from its liver storage form.30
Glucose is stored in the liver and muscle for release during periods of fasting and exercise.
Inhibiting the enzyme glycogen phosphorylase blocks excess glucose release into the bloodstream.
When fed to diabetic mice, clove extracts significantly suppressed blood glucose elevations and hemoglobin A1c (HbA1c), which is an indicator of chronic glucose levels.30
In order to assess the potential effectiveness of water-soluble clove extract in reducing postprandial glucose spikes, researchers assembled a group of human volunteers. These study subjects were classified according to their baseline levels into normal and high-glucose groups.5
In this open-label study, all subjects received 250 mg of a water-soluble clove extract once daily for 30 days.
Random blood glucose levels were measured prior to supplementation on day 1, and then on days 12, 24, and 30. Additional blood draws were done two hours following a typical lunch (no special diet was provided).
Results from this study showed that in the normal- and high-baseline blood-glucose groups, postprandial glucose measurements fell significantly at day 12 and continued to fall throughout the study, to nearly the same level as the before-meal values.5
Stated differently, in response to the clove extract supplement, after-meal glucose levels dropped to about the same level as before-meal values (See Figure 3).
In the group that had the higher baseline blood-glucose levels, the amount of postprandial glucose decreases was greater than in the normal group, indicating a more powerful effect in this at-risk population.5
At the same time, no subject experienced abnormally low blood-glucose levels, an important safety feature, especially in comparison with many prescription glucose-lowering drugs that can cause hypoglycemia (low blood sugar).
Figure 3: Clove Extract Reduces After-Meal Blood Glucose in Humans
 |
 |
Two groups of people were studied for 30 days. Group I had normal after-meal glucose. Group II had high after-meal glucose. Daily intake of 250 mg of water-soluble clove extract reduced after-meal glucose levels by 21.5% in Group I and by 27.1% in Group II.
Summary

Although most mainstream physicians still look at fasting blood glucose as the primary indicator of a person’s sugar-related risk, the published scientific literature increasingly points to other measures—especially postprandial glucose and insulin—as important and sensitive data points.
Elevated glucose and insulin levels two hours after a meal are known to indicate risk related to development of type II diabetes and cardiovascular disease.
In fact, postprandial (after-meal) blood glucose can be high and dangerous even in people with normal fasting glucose levels.
This means that everyone—not just those with known elevations in fasting glucose—needs to be alert to postprandial glucose and insulin spikes, and take necessary steps to address metabolic dysfunction.
That’s where supplementation with standardized maqui-berry and water-soluble clove extracts comes in.
Both extracts have been shown in human studies to significantly lower blood glucose, each through a different and complementary mechanism. In addition, maqui-berry extract has also demonstrated important insulin lowering abilities.
Both can be used to keep postprandial blood glucose and insulin in safer ranges, potentially adding years of high-quality life in diabetics, prediabetics, and non-diabetics alike.
Supplementation with standardized maqui-berry and water-soluble clove extracts just once per day is a sensible approach to maintaining metabolic health.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
Fasting vs. Postprandial (After-Meal) Glucose Elevations
 |
As long ago as 1983, it was evident that nondiabetic older adults with fasting blood glucose levels similar to those of younger people regularly “failed” a glucose tolerance test.31
A glucose tolerance test measures blood glucose both at a fasting baseline, and then again two hours after a standardized glucose drink, and is an indicator of how well the body can manage a large quantity of glucose.
To pass this test, blood glucose should not rise above 140 mg/dL at the two-hour mark, indicating both potent pancreatic insulin secretion and vigorous uptake of glucose from the blood by insulin-stimulated cellular mechanisms.32
Postprandial blood-glucose levels above 140 and below 200 mg/dL are one indication of so-called prediabetes, a condition in which most of the risk factors for diabetes and its complications, including cardiovascular disease, are gradually rising.7
Another way of evaluating overall blood-glucose handling in the body is to measure the proportion of glucose that has become “stuck” to hemoglobin protein, which is called hemoglobin A1c, or HbA1c.
The normal value for HbA1c is 5.6% or lower, while a level of 6.5% or greater is an indicator of diabetes if found on two separate occasions.33
Levels between 5.6% and 6.5% are another way of defining prediabetes.33
According to 2012 public health data, 51% of Americans over 65 years of age are prediabetic, based on fasting blood glucose or HbA1c.34
References
- Gerich JE. Clinical significance, pathogenesis, and management of postprandial hyperglycemia. Arch Intern Med. 2003;163(11): 1306-16.
- Madsbad S. Impact of postprandial glucose control on diabetes-related complications: How is the evidence evolving? J Diabetes Complications. 2016;30(2):374-85.
- Fowler GC, Vasudevan DA. Type 2 diabetes mellitus: managing hemoglobin A(1c) and beyond. South Med J. 2010;103(9):911-6.
- Hidalgo J, Flores C, Hidalgo MA, et al. Delphinol(R) standardized maqui berry extract reduces postprandial blood glucose increase in individuals with impaired glucose regulation by novel mechanism of sodium glucose cotransporter inhibition. Panminerva Med. 2014;56(2 Suppl 3):1-7.
- Supplier Internal Study. Effect of Clovinol on Random Blood Sugar Levels - A Pilot Study. Data on File. 2017.
- Avogaro A. Postprandial glucose: marker or risk factor? Diabetes Care. 2011;34(10):2333-5.
- Guclu M, Ali A, Eroglu DU, et al. Serum Levels of sRAGE Are Associated with Body Measurements, but Not Glycemic Parameters in Patients with Prediabetes. Metab Syndr Relat Disord. 2016;14(1):33-9.
- Barlovic DP, Thomas MC, Jandeleit-Dahm K. Cardiovascular disease: what’s all the AGE/RAGE about? Cardiovasc Hematol Disord Drug Targets. 2010;10(1):7-15.
- Csiszar A, Ungvari Z. Endothelial dysfunction and vascular inflammation in type 2 diabetes: interaction of AGE/RAGE and TNF-alpha signaling. Am J Physiol Heart Circ Physiol. 2008;295(2):H475-6.
- Ning F, Tuomilehto J, Pyorala K, et al. Cardiovascular disease mortality in Europeans in relation to fasting and 2-h plasma glucose levels within a normoglycemic range. Diabetes Care. 2010;33(10):2211-6.
- Kato M, Tani T, Terahara N, et al. The Anthocyanin Delphinidin 3-Rutinoside Stimulates Glucagon-Like Peptide-1 Secretion in Murine GLUTag Cell Line via the Ca2+/Calmodulin-Dependent Kinase II Pathway. PLoS One. 2015;10(5):e0126157.
- Imeryuz N, Yegen BC, Bozkurt A, et al. Glucagon-like peptide-1 inhibits gastric emptying via vagal afferent-mediated central mechanisms. Am J Physiol. 1997;273(4 Pt 1):G920-7.
- Näslund E, Bogefors J, Skogar S, et al. GLP-1 slows solid gastric emptying and inhibits insulin, glucagon, and PYY release in humans. Am J Physiol. 1999;277(3 Pt 2):R910-6.
- Geser CA. Hormonal interactions in carbohydrate metabolism. Int Z Vitam Ernahrungsforsch Beih. 1976;15:58-65.
- Niswender KD. Basal insulin: physiology, pharmacology, and clinical implications. Postgrad Med. 2011;123(4):17-26.
- Wilcox G. Insulin and insulin resistance. Clin Biochem Rev. 2005;26(2):19-39.
- Chu NF, Spiegelman D, Hotamisligil GS, et al. Plasma insulin, leptin, and soluble TNF receptors levels in relation to obesity-related atherogenic and thrombogenic cardiovascular disease risk factors among men. Atherosclerosis. 2001;157(2):495-503.
- Burnol AF, Morzyglod L, Popineau L. [Cross-talk between insulin signaling and cell proliferation pathways]. Ann Endocrinol (Paris). 2013;74(2):74-8.
- Nilsen TI, Vatten LJ. Prospective study of colorectal cancer risk and physical activity, diabetes, blood glucose and BMI: exploring the hyperinsulinaemia hypothesis. Br J Cancer. 2001;84(3):417-22.
- Balkau B, Kahn HS, Courbon D, et al. Hyperinsulinemia predicts fatal liver cancer but is inversely associated with fatal cancer at some other sites: the Paris Prospective Study. Diabetes Care. 2001;24(5):843-9.
- Godsland IF, Crook D, Walton C, et al. Influence of insulin resistance, secretion, and clearance on serum cholesterol, triglycerides, lipoprotein cholesterol, and blood pressure in healthy men. Arterioscler Thromb. 1992;12(9):1030-5.
- Salonen JT, Lakka TA, Lakka HM, et al. Hyperinsulinemia is associated with the incidence of hypertension and dyslipidemia in middle-aged men. Diabetes. 1998;47(2):270-5.
- Mykkanen L, Kuusisto J, Haffner SM, et al. Hyperinsulinemia predicts multiple atherogenic changes in lipoproteins in elderly subjects. Arterioscler Thromb. 1994;14(4):518-26.
- Karhapaa P, Malkki M, Laakso M. Isolated low HDL cholesterol. An insulin-resistant state. Diabetes. 1994;43(3):411-7.
- Ko GT, Cockram CS, Woo J, et al. Obesity, insulin resistance and isolated low high-density-lipoprotein cholesterol in Chinese subjects. Diabet Med. 2001;18(8):663-6.
- Goldstein BJ. Insulin resistance as the core defect in type 2 diabetes mellitus. Am J Cardiol. 2002;90(5a):3g-10g.
- Modan M, Halkin H, Almog S, et al. Hyperinsulinemia. A link between hypertension obesity and glucose intolerance. J Clin Invest. 1985;75(3):809-17.
- Speakman JR, Goran MI. Tissue-specificity and ethnic diversity in obesity-related risk of cancer may be explained by variability in insulin response and insulin signaling pathways. Obesity (Silver Spring). 2010;18(6):1071-8.
- Alvarado J, Schoenlau F, Leschot A, et al. Delphinol(R) standardized maqui berry extract significantly lowers blood glucose and improves blood lipid profile in prediabetic individuals in three-month clinical trial. Panminerva Med. 2016;58(3 Suppl 1):1-6.
- Sanae F, Kamiyama O, Ikeda-Obatake K, et al. Effects of eugenol-reduced clove extract on glycogen phosphorylase b and the development of diabetes in db/db mice. Food & Function. 2014;5(2): 214-9.
- Fink RI, Kolterman OG, Griffin J, et al. Mechanisms of Insulin Resistance in Aging. Journal of Clinical Investigation. 1983;71(6): 1523-35.
- Yanase M, Takatsu F, Tagawa T, et al. Insulin resistance and fasting hyperinsulinemia are risk factors for new cardiovascular events in patients with prior coronary artery disease and normal glucose tolerance. Circ J. 2004;68(1):47-52.
- Available at: http://www.mayoclinic.org/tests-procedures/a1c-test/details/results/rsc-20167939. Accessed 19 April, 2017.
- Available at: https://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed July 7, 2017.
- Kakehi E, Kotani K, Nakamura T, et al. Non-diabetic Glucose levels and Cancer Mortality: A Literature Review. Curr Diabetes Rev. 2017.

