Life Extension Magazine®
Vitamin D is best known for bone health, but its potential role in cancer prevention has made it one of the most popular supplements today.
A recent study reveals a new benefit of vitamin D: metabolic health.
In a new article, Italian scientists reviewed previous studies on vitamin D and found a connection to bone and metabolic health.
In their review of the literature, the researchers showed strong associations between inadequate vitamin D levels and inflammation, osteoporosis, insulin resistance, and type II diabetes.1
The scientists concluded that vitamin D may become an important therapeutic agent in the fight against metabolic disease, as well as disorders caused by inflammation.
What you need to know
- Vitamin D is both vitamin and hormone, with wide-ranging effects throughout the human body.
- For years, vitamin D was known for its role in promoting calcium absorption for healthy bones.
- More recent studies have revealed that vitamin D has potent anti-inflammatory properties important to osteoporosis prevention that are distinct from its role in promoting calcium absorption.
- Those same anti-inflammatory properties have been shown to be effective at preventing and mitigating metabolic disturbances, particularly insulin resistance and type II diabetes.
- Human studies show that vitamin D supplementation is particularly effective in people with blood sugar and other metabolic abnormalities and low baseline vitamin D levels.
- Such studies demonstrate why higher doses of vitamin D are required for metabolic control.
- Studies like these make it clear that getting an annual vitamin D blood level, and supplementing as needed with vitamin D3, provides a multitargeted effect on both bone and metabolic health.
Vitamin D: The Bone Vitamin
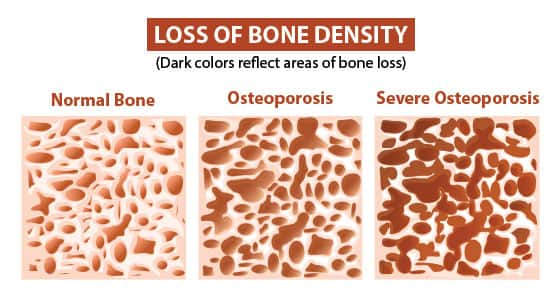
For older individuals, vitamin D deficiency contributes to osteoporosis and higher fracture risk.2-4 Educated seniors supplement with vitamin D and other nutrients to reduce their loss of bone density.
Vitamin D has anti-inflammatory properties that are also important when it comes to preventing osteoporosis.
In recent years, we have come to understand that osteoporosis is an inflammation-driven condition.2,6-8
Inflammation disrupts the delicate balance between bone breakdown (resorption) and bone formation, favoring resorption and slowing new bone formation.2
Today, it is recognized that people with chronic inflammatory conditions generally have weaker, less well-mineralized bones than healthy adults of the same age—a clear-cut demonstration of the role of inflammation in bone health.6,7
Vitamin D works in multiple ways to rein in the immune system’s excessive inflammatory responses. This makes it clear that vitamin D provides far more comprehensive bone support than simply enhancing calcium absorption.
These findings reveal vitamin D to be a modulator of inflammation as a means of preserving bone strength.1
It opens the door to other important roles for vitamin D.
Vitamin D and Metabolic Changes
Vitamin D is a hormone that has specific receptors that trigger structural, functional, and metabolic changes throughout the body. It is vitamin D’s role as a steroid-like hormone that triggered research that brings together the impact of inflammation on both bone and metabolic health.
This research pointed out previous studies that showed vitamin D’s multiple actions on blood sugar and other metabolic factors. These studies show that vitamin D deficiency is implicated in a low-grade, chronic inflammatory state associated with insulin resistance, metabolic syndrome, and the risk of developing type II diabetes.1
Even in nondiabetics, lower vitamin D levels correlate with poorer insulin responsiveness, meaning less control over blood sugar.1 Low plasma vitamin D levels are also closely correlated with higher body mass index (BMI), fat mass, and waist circumference.1
But correlation between nutrient status and health status does not prove a cause-and-effect relationship. Clinical trials are required to establish that kind of connection—and that’s exactly what we’ll examine next.
Vitamin D’s Role in Blood-Sugar Control

Studies have repeatedly shown that when animals are vitamin D deficient, supplementation with the vitamin reduces inflammation and improves insulin sensitivity.1
Human studies have also shown that vitamin D supplementation is effective at managing blood sugar and other metabolic abnormalities—especially in people with low vitamin D levels.
In type II diabetics who were vitamin D deficient (blood levels less than 20 ng/mL), taking 1,000 IU/day of vitamin D3 led to improvements in endothelial function, improved measures of glucose-related protein damage (glycation), as well as in other markers of blood-vessel health.9
Proper dosing is especially important. For example, studies using just 400 or 800 IU/day of vitamin D3 showed neither a reduction in diabetes incidence nor any change in blood-sugar levels,10,11 whereas in subjects with low baseline vitamin D levels, higher doses of vitamin D proved highly effective.
In a study of subjects with low vitamin D3, providing 4,000 IU/day of D3 led to significant improvements in insulin sensitivity and favorable reductions in fasting insulin levels.12
Perhaps the most compelling data on vitamin D use in supporting metabolic health comes from studies looking expressly at people at risk for type II diabetes, or prediabetics.1 Such people have impaired fasting glucose (fasting sugar levels between 100 and 125 mg/dL), or impaired glucose tolerance (an abnormal rise in blood sugar following a metered dose of oral glucose).
Studies in these populations now show that supplementing with vitamin D3 daily slowed the rise in fasting blood sugar over time, improved pancreatic insulin secretion, and boosted insulin sensitivity.13,14
Additional Mechanisms of Action
Vitamin D also has a direct impact on insulin sensitivity and resistance independent of its anti-inflammatory effect.1 Studies show that vitamin D triggers increased insulin sensitivity and lowers blood sugar by at least three complementary mechanisms:
• Interactions with vitamin D receptors on skeletal muscle, where it may help to trigger maturation of developing glucose-hungry muscle cells.15
• Increased expression of insulin receptors on cells throughout the body. Those receptors in turn promote glucose transport from blood into cells.1
• Activation of a molecular complex called PPAR-delta, which regulates genes involved in burning sugar and fat for energy.1
Multiple other mechanisms by which vitamin D stimulates the transfer of sugar from blood into cells are gradually coming to light, including complex interactions with other hormone systems. It even appears to directly stimulate the pancreas to release insulin.1
Vitamin D and Inflammation
Vitamin D was once thought of primarily for its role in bone health by promoting calcium absorption. More recently, it has been found to play an unexpected but important role in modulating immunity and inflammation.1
This property reveals two important facts:
- Vitamin D is doubly important in osteoporosis, since we now know that inflammation plays a role in the bone condition.
- It highlights vitamin D’s value as an essential actor in maintaining body-wide metabolic health.
Studies show that vitamin D suppresses the inflammation generated by fat tissue.
Under the influence of vitamin D, immune cells increase their production of anti-inflammatory cytokines, while reducing levels of pro-inflammatory cytokines.1 Vitamin D has similar effects on cells called lymphocytes that are involved in regulating immune responses: It shifts their profile from an inflammation-promoting to an inflammation-suppressing one.
Vitamin D acts on immune system cell receptors, where binding to the vitamin triggers regulation of more than 1,000 genes.1 These gene-regulatory properties likely account for vitamin D’s favorable effects on emerging cancer cells.
Inflammation is considered the “final common pathway” for numerous age-related disorders. The discovery of vitamin D’s anti-inflammatory actions means we can expect to see more studies widening the applications of vitamin D beyond preventing osteoporosis and diabetes, to its role in other chronic, inflammation-driven conditions that shorten lifespan and promote disease.
Summary

Vitamin D arrived on the medical scene more than a century ago, and was largely viewed as the “calcium and bone vitamin.”
Recent studies show that such a view overly simplifies both bone health and vitamin D’s roles in the human body.
We now recognize that osteoporosis is an inflammatory disorder as much as it is a calcium-related disorder. We also now understand that vitamin D’s anti-inflammatory actions contribute as much to its anti-osteoporosis actions as its calcium-promoting properties.
Finally, the anti-inflammatory actions of vitamin D cross over from improving bone to maintaining healthy metabolic status by supporting normal insulin action and suppressing elevated blood sugar.
The human body is a miracle of interacting systems with unexpected relationships. Our new knowledge about vitamin D further highlights these surprising connections, and amplifies the case for maintaining ample vitamin D levels as we age.
For vitamin D, the typical dose range is 3,000 IU to 8,000 IU daily, taken with a meal for better absorption.
Annual blood tests can enable one to know if they are taking the proper dose of vitamin D they need to achieve optimal levels.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
References
- Garbossa SG, Folli F. Vitamin D, sub-inflammation and insulin resistance. A window on a potential role for the interaction between bone and glucose metabolism. Rev Endocr Metab Disord. 2017;18(2):243-58.
- Al-Daghri NM, Yakout S, Al-Shehri E, et al. Inflammatory and bone turnover markers in relation to PTH and vitamin D status among saudi postmenopausal women with and without osteoporosis. Int J Clin Exp Med. 2014;7(10):3528-35.
- Mata-Granados JM, Cuenca-Acevedo JR, Luque de Castro MD, et al. Vitamin D insufficiency together with high serum levels of vitamin A increases the risk for osteoporosis in postmenopausal women. Arch Osteoporos. 2013;8:124.
- Peris P, Martinez-Ferrer A, Monegal A, et al. 25 hydroxyvitamin D serum levels influence adequate response to bisphosphonate treatment in postmenopausal osteoporosis. Bone. 2012;51(1):54-8.
- Wolf G. The discovery of vitamin D: the contribution of Adolf Windaus. J Nutr. 2004;134(6):1299-302.
- Bastos CM, Araujo IM, Nogueira-Barbosa MH, et al. Reduced bone mass and preserved marrow adipose tissue in patients with inflammatory bowel diseases in long-term remission. Osteoporos Int. 2017;28(7):2167-76.
- Gallo J, Raska M, Kriegova E, et al. Inflammation and its resolution and the musculoskeletal system. J Orthop Translat. 2017;10:52-67.
- Lin SY, Hsu WH, Lin CC, et al. Effect of acute pancreatitis on the risk of developing osteoporosis: A nationwide cohort study. PLoS One. 2017;12(6):e0179358.
- Shab-Bidar S, Neyestani TR, Djazayery A, et al. Regular consumption of vitamin D-fortified yogurt drink (Doogh) improved endothelial biomarkers in subjects with type 2 diabetes: a randomized double-blind clinical trial. BMC Med. 2011;9:125.
- Avenell A, Cook JA, MacLennan GS, et al. Vitamin D supplementation and type 2 diabetes: a substudy of a randomised placebo-controlled trial in older people (RECORD trial, ISRCTN 51647438). Age Ageing. 2009;38(5):606-9.
- de Boer IH, Tinker LF, Connelly S, et al. Calcium plus vitamin D supplementation and the risk of incident diabetes in the Women’s Health Initiative. Diabetes Care. 2008;31(4):701-7.
- von Hurst PR, Stonehouse W, Coad J. Vitamin D supplementation reduces insulin resistance in South Asian women living in New Zealand who are insulin resistant and vitamin D deficient - a randomised, placebo-controlled trial. Br J Nutr. 2010;103(4):549-55.
- Mitri J, Dawson-Hughes B, Hu FB, et al. Effects of vitamin D and calcium supplementation on pancreatic beta cell function, insulin sensitivity, and glycemia in adults at high risk of diabetes: the Calcium and Vitamin D for Diabetes Mellitus (CaDDM) randomized controlled trial. Am J Clin Nutr. 2011;94(2):486-94.
- Nazarian S, St Peter JV, Boston RC, et al. Vitamin D3 supplementation improves insulin sensitivity in subjects with impaired fasting glucose. Transl Res. 2011;158(5):276-81.
- Simpson RU, Thomas GA, Arnold AJ. Identification of 1,25-dihydroxyvitamin D3 receptors and activities in muscle. J Biol Chem. 1985;260(15):8882-91.

