Hearing Loss
Hearing Loss
Last Section Update: 05/2023
Contributor(s): Maureen Williams, ND; Shayna Sandhaus, PhD; Stephen Tapanes, PhD; Chancellor Faloon, Health & Wellness Author
Table of Contents
- Overview
- What are the Types of Hearing Loss?
- Nutrients
- Dietary & Lifestyle Considerations
- Hearing Loss Causes and Risk Factors
- How is Hearing Loss Assessed and Diagnosed?
- Treatment of Hearing Loss
- Novel and Emerging Hearing Loss Treatment Approaches
- The Consequences of Untreated Hearing Loss
- Hearing Loss: Frequently Ask Questions
- Update History
- References
1 Overview
Hearing Loss: Summary and Quick Facts
- Most people will experience some form of hearing loss during their lifetime.
- Hearing loss affects almost 14% of people aged 45–64 years and almost 27% of those aged 65 and over.1 However, people of all ages can experience hearing loss.2
- Young people are at increasing risk of hearing loss due to the ubiquity of personal listening devices and listening to music too loud.3
- People with hearing loss spend more money on healthcare than those without hearing loss.4
- Fortunately, many effective hearing loss treatment options are available, including more widely accessible and effective hearing aids.
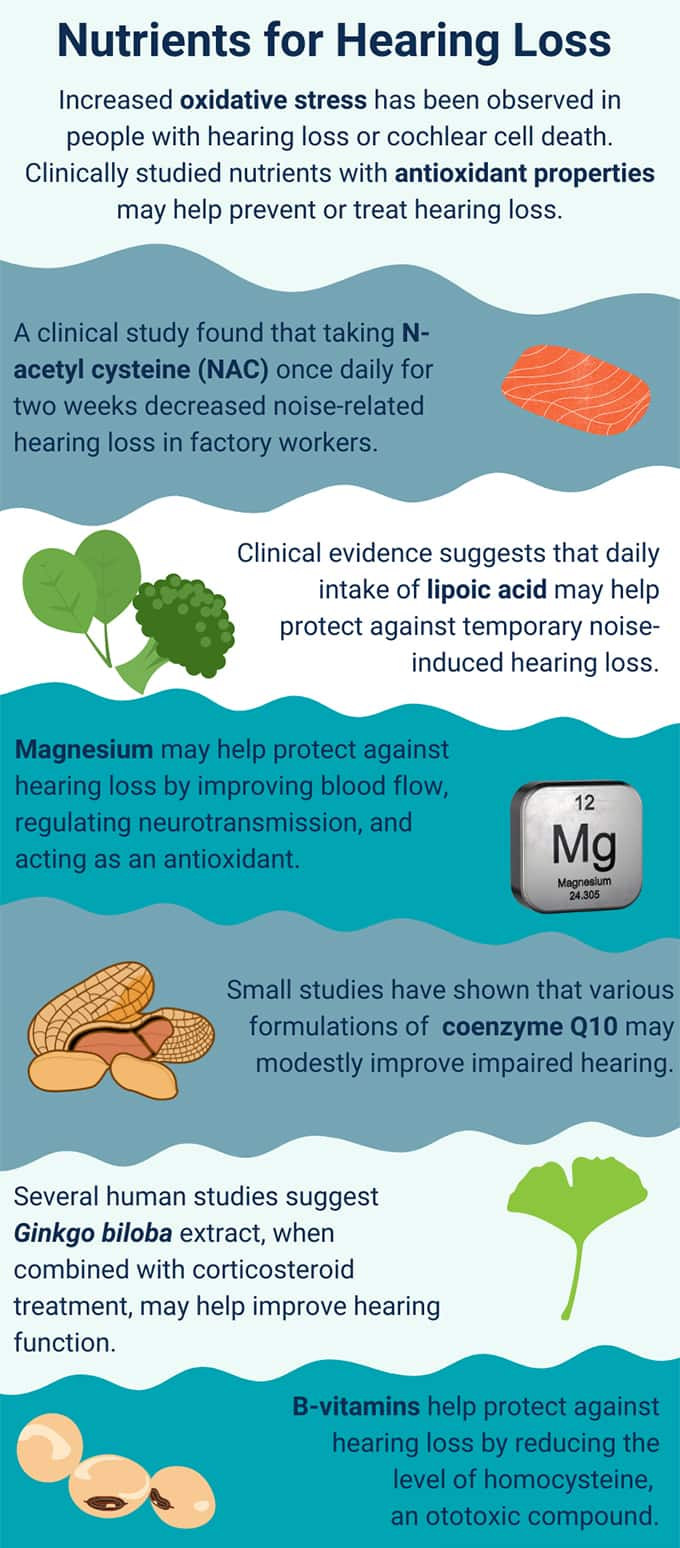
- Several nutrients may support hearing health as well, including magnesium, N-acetyl cysteine, and lipoic acid.
2 What are the Types of Hearing Loss?
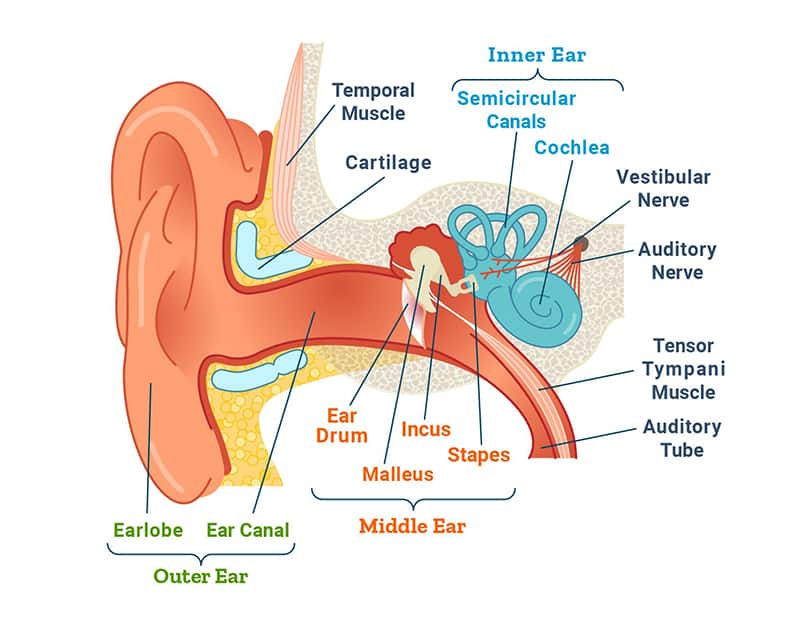
There are three types of hearing loss: sensorineural, conductive, and mixed hearing loss (a combination of conductive and sensorineural). The type of hearing loss is determined by whether the outer, middle, or inner ear is affected. Outer ear problems cause conductive hearing loss, whereas inner ear damage results in sensorineural hearing loss.5
To better understand the three types of hearing loss, it is important to understand the anatomy of the ear. The ear is divided into three areas6,7:
- The outer ear, which comprises the external ear (auricle) and ear canal
- The middle ear, which consists of the ear drum (tympanic membrane) and the three hearing bones (the ossicles: malleus, incus, and stapes)
- The inner ear, which comprises the cochlea, balance organs (saccule, utricle, and semicircular canals), vestibular and facial nerves, and internal auditory canal.
The auricle funnels sound waves into the external auditory canal. At the end of that canal, the sound waves vibrate the tympanic membrane. This vibration then causes the ossicles to move, and ultimately shifts fluids within the cochlea. These fluid shifts activate hearing cells in the cochlea (outer and inner hair cells which are the cells responsible for converting the mechanical energy of sound waves into electrical energy) and cause electrical signals to travel from the cochlea to the brain, thereby giving rise to the perception of sound.8
Sensorineural Hearing Loss
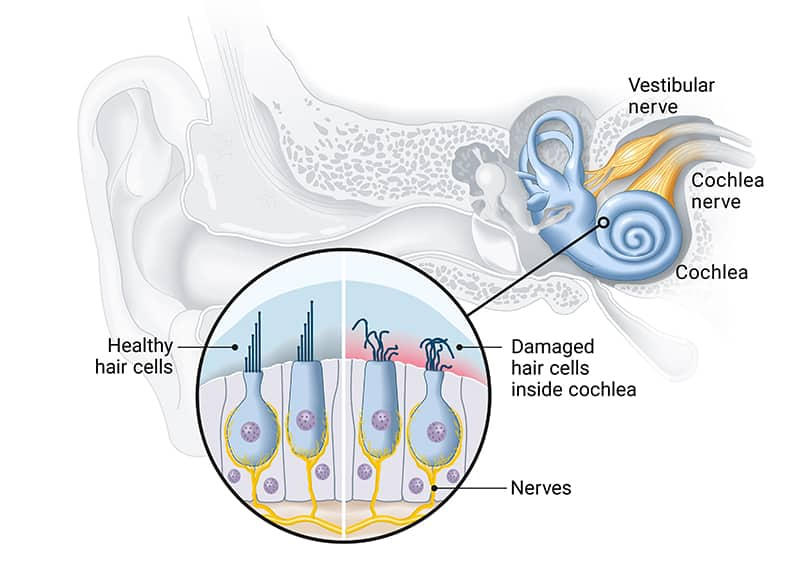
Sensorineural hearing loss accounts for the majority of all cases of hearing loss.9 Damage to the inner ear or auditory nerve is usually responsible and causes progressive hearing loss. The most common type of sensorineural hearing loss, presbycusis, or age-related hearing loss (ARHL), is sensorineural in origin. It is marked by the gradual loss of high-frequency hearing on both sides in elderly individuals. Age-related hearing loss is also associated with tinnitus (ie, ringing in the ears).10
The second-most-common type of sensorineural hearing loss is noise-induced. The mechanical impact of sound waves on the hair cells of the cochlea can, when excessive and/or recurring, cause cell death. This type of hearing loss is highly preventable.10,11
Certain medications are toxic to the organs of the inner ears (ototoxic) and can cause sensorineural hearing loss by damaging auditory tissues.12 Sensorineural hearing loss can also be due to Ménière disease, a condition also characterized by dizzy spells and tinnitus, and thought to be caused by dysregulation of inner ear pressure.13,14
Conductive Hearing Loss
Conductive hearing loss occurs when sound does not properly reach the inner ear. Common causes include infection that leads to middle ear or eustachian tube blockage, blockage from fluid or earwax, trauma, tumors, or fixation of the bones of the middle ear (eg, otosclerosis). Otitis media, an infection of the middle ear, can cause temporary, usually mild, hearing loss. It is common in children but also occurs in adults. Serous otitis media is an aftermath of acute infection in which thick fluid remains in the middle ear for a protracted period. In sinusitis, other upper respiratory tract infections, and allergies, the eustachian tube can become blocked, resulting in hearing loss. Infections causing hearing loss tend to occur more often in children and young adults. Blockage by earwax can occur at any age and accounts for many cases of apparent hearing loss.8,15,16
3 Nutrients
Targeting Reactive Oxygen Species
Reactive oxygen species (free radicals) are involved in a wide range of health concerns, including the development and progression of hearing loss. Increased oxidative stress has been demonstrated in people with unexplained sudden sensorineural hearing loss, and oxidative stress contributes to cochlear cell death.17,18 Antioxidants, which are compounds that have the ability to neutralize damaging oxidative stress, are a promising therapeutic strategy to prevent and treat hearing loss.19,20 In fact, oxidative stress-reducing agents have been widely studied for the prevention and treatment of hearing loss due to drug-induced ear damage (ototoxicity).17 Preclinical evidence suggests the most important role for antioxidants may be in hearing loss prevention.19
N-acetyl cysteine (NAC) increases the production of glutathione, one of the most important antioxidants in the body.21 NAC also acts as a direct free radical scavenger, which may contribute to its potential usefulness in preventing and treating hearing loss.22,23
A randomized placebo-controlled trial in 566 military personnel found NAC prevented some noise-induced hearing changes during weapons training, although the effects were not statistically significant.24 Another randomized controlled trial in 48 textile workers regularly exposed to loud noise found 1,200 mg NAC per day for 14 days decreased temporary noise-related hearing loss.25 In a controlled trial in 41 patients with sudden sensorineural hearing loss, those who received NAC along with intratympanic (through the eardrum) injections of the steroid dexamethasone for 14 days gained an ability to hear a specific high pitch (8,000 Hz) and were more likely to recover their hearing than those who received intratympanic steroid injections alone.26 Observational data from 219 patients with sudden sensorineural hearing loss indicated adding NAC to standard oral corticosteroid therapy may improve some aspects of hearing recovery.27
Lipoic acid has received research attention for its possible role in preventing and treating hearing loss, and has shown promise in preclinical models of age-related, noise-induced, and ototoxic drug-related hearing loss.28-31 Clinical trials of alpha-lipoic acid have also shown promise. A controlled trial that included 30 healthy volunteers with normal hearing found 600 mg lipoic acid daily for 10 days prior to experimental noise exposure reduced temporary noise-induced hearing loss better than a single 600 mg dose of lipoic acid one hour before noise exposure or no lipoic acid.32 In a clinical trial in 46 elderly subjects with age-related hearing loss, treatment with 60 mg lipoic acid, 600 mg vitamin C, and 300 mg rebamipide (a pharmaceutical antioxidant not currently available in the United States) per day for at least eight weeks significantly improved hearing at all frequencies tested.33
Greater consumption of vitamins A, C, and E appears to be associated with reduced risk of age-related hearing loss.34 This effect may be mediated in part via protection of hair cells from oxidative damage, as shown in one rat study in which supplementation with vitamins A, C, and E, along with magnesium, helped mitigate hair cell death following noise-induced hearing loss.35 Higher dietary consumption of vitamins A and E was found to be associated with a lower prevalence of hearing loss in an observational study of a population of nearly 3,000 adults over 50 years of age.36 Beta-carotene, vitamin C and vitamin E intakes, as well as magnesium intake, were all associated with lower risk of hearing loss in an observational study that included data from 2,592 U.S. adults. The study also found beta-carotene, vitamin C, and vitamin E had a stronger relationship with hearing preservation as a group than as individual nutrients.37 A systematic review that included three clinical trials with a total of 279 participants found incorporating antioxidant therapy with vitamins A, C, and E into treatment of sudden sensorineural hearing loss led to enhanced hearing gains.38 In one controlled clinical trial, 70 patients with sudden unexplained sensorineural hearing loss were treated with 7,800 mcg RAE (26,000 IU) beta-carotene (pro-vitamin A), 200 mg vitamin C, 90 mg (200 IU) vitamin E (d-alpha tocopherol), and 50 mcg of the mineral selenium twice daily as an adjunct to medical therapy as well as hyperbaric oxygen, while 56 similar patients received medical and hyperbaric oxygen therapies alone, for 30 days. Both groups experienced hearing improvement, but those receiving the antioxidant supplements had greater improvement.39
Coenzyme Q10 (CoQ10) is an antioxidant that plays a vital role in cellular metabolism and energy production. A number of animal studies indicated CoQ10 can lower oxidative stress in auditory system tissues and protect against hearing loss due to aging, noise exposure, and ototoxic drugs.40-44 In an uncontrolled trial in 18 volunteers, 30 days of treatment with a water-soluble form of CoQ10 shortened the time to hearing recovery after experimental noise exposure.45 A placebo-controlled trial that included 60 participants with age-related hearing loss found 30 days of treatment with 160 mg of water-soluble CoQ10 daily resulted in hearing gains at mid-range and higher frequencies compared with 50 mg per day of vitamin E or placebo.46
An observational study found 30 individuals with unexplained sudden sensorineural hearing loss had lower CoQ10 levels than 60 similar subjects with healthy hearing.47 In a trial in which 120 patients with sudden sensorineural hearing loss were treated with systemic steroids alone or combined with CoQ10, both treatment approaches resulted in hearing improvement, but steroids plus CoQ10 led to greater improvement in speech discrimination.48
Zinc, a mineral involved in many physiological processes (including nervous system function), is present in significant amounts in the cochlea of the inner ear. It is a component of one of the body’s critical endogenous antioxidant enzymes and thus helps protect the delicate inner-ear tissues from oxidative damage.49 A randomized controlled trial that enrolled 66 participants with sudden sensorineural hearing loss compared corticosteroid treatment plus 78 mg oral zinc gluconate (providing 20 mg of elemental zinc) daily to corticosteroids alone. The zinc group experienced greater hearing gain and a higher likelihood of recovery, and the degree of hearing improvement was correlated with the amount of increase in blood zinc levels.50
Methionine is an amino acid needed to produce glutathione. In a small, exploratory, randomized, placebo-controlled trial that included 27 cancer patients being treated with a chemotherapy agent known to cause ototoxicity, those given oral D-methionine (100 mg per kg of bodyweight) along with chemotherapy were protected from drug-induced hearing loss.51 Studies in animals also indicate D-methionine supplementation may help prevent noise-induced hearing loss, particularly when taken before or within 36–72 hours after exposure, and may protect against drug-related ototoxicity.52-55
Magnesium
Insufficient magnesium intake and suboptimal blood and cellular magnesium levels are common.56,57 This problem has been associated with high rates of cardiovascular disease, diabetes, high blood pressure, and other chronic conditions. Magnesium also plays an important role in inflammatory and oxidative processes.58,59 Magnesium may protect against hearing loss through several mechanisms, including its abilities to counteract excessive calcium concentrations, improve blood flow by promoting vasodilation, exert antioxidant effects, and help regulate excitatory neurotransmission.60
In one double-blind study published in 1993, a group of 320 military personnel were given about 160 mg of elemental magnesium (in the form of magnesium aspartate) or a placebo on most days for two months. At the end of the trial, permanent hearing loss occurred twice as often in the placebo group as the magnesium group.61 In a similar study by the same research group, 300 young, healthy military recruits received the same magnesium formulation during firearms training. This study found that magnesium supplementation increased red blood cell magnesium concentrations, and that some measures of hearing loss inversely correlated with red blood cell magnesium status. In other words, hearing loss was less prevalent in the participants with higher red blood cell magnesium.62 A controlled clinical trial conducted in Israel and published in 2002 enrolled 133 participants with unexplained sudden hearing loss. The study subjects were treated with either a combination of intravenous magnesium with carbogen inhalation (ie, a gaseous mixture of 5% CO2 and 95% O2 that causes vasodilation when inhaled) therapy or carbogen inhalation alone. Carbogen may be helpful in cases of sudden hearing loss by increasing blood flow to the inner ear. In the study, the addition of intravenous magnesium resulted in a higher rate of hearing recovery.63
In a randomized controlled trial, 51 cochlear implant recipients were given a daily combination of 315 mg magnesium plus 18 mg beta-carotene, 500 mg vitamin C, and 267 mg vitamin E (dl-alpha-tocopherol) or placebo orally for 106 days. Those who received magnesium plus antioxidants were found to have better hearing preservation over a three-month period than those who received placebo. The difference amounted to an 8 decibel (dB) hearing loss reduction among those who received the antioxidants and magnesium.64 An observational study in nearly 2,600 participants, aged 20–69 years, found greater intakes of magnesium, beta-carotene, vitamin C, and vitamin E, were each associated with better hearing of speech and high frequencies.37
Ginkgo Biloba
Ginkgo biloba standardized extract has been extensively studied for its possible benefits in age-related conditions like cognitive impairment and dementia.65-67 Numerous controlled clinical trials have been undertaken in individuals with sudden sensorineural hearing loss. A meta-analysis of findings from 11 randomized controlled trials with a total of 1,069 participants found ginkgo extract may be beneficial when combined with corticosteroid therapy as initial treatment in patients with sudden sensorineural hearing loss, but more high-quality research is needed to conclusively establish ginkgo’s effects in patients with this condition.68
One observational study reviewed outcomes in 56 patients with unilateral sudden sensorineural hearing loss, 30 of whom received ginkgo extract as part of their treatment. In those with profound hearing loss, the addition of ginkgo to conventional intravenous corticosteroid therapy restored hearing to a significantly greater degree than the steroid treatment alone.69
Likely mechanisms for these benefits include ginkgo’s well-established ability to combat oxidative stress through stimulating antioxidant enzyme activity, reducing reactive free radicals, and decreasing lipid peroxidation,70 as well as possibly preventing noise-induced damage to cochlear synapses.71
B-Vitamins and Homocysteine
Folate and vitamin B12 are necessary for normal function of cells throughout the body, including nerve cells. These vitamins also help reduce levels of homocysteine, a potentially toxic compound that builds up in the body when B12, folate, and other nutrient levels are low. Elevated homocysteine levels are linked to increased risks of cardiovascular disease, stroke, and dementia, as well as heart disease-related death.72,73 Blood vessel dysfunction is an important pathologic consequence of elevated homocysteine levels and a known cause of cardiovascular disease.74,75 Some data suggest vascular dysfunction and other negative influences on blood vessel health also play a role in sensorineural hearing loss.18,76,77
In a randomized placebo-controlled trial in 20 healthy volunteers aged 20‒30 years, a 1 mg vitamin B12 injection daily for seven days followed by a 5 mg injection on day eight protected against experimental noise-induced hearing loss.78 In an observational study involving close to 3,000 adults over age 50, there was a 64% increased prevalence of hearing loss among individuals with extremely high serum homocysteine levels (>20 micromoles/liter), and a 37% increased prevalence in those with low serum folate levels.79 Another observational study similarly found low folate levels were correlated with age-related hearing loss, while in an animal model, folate deficiency was found to precipitate premature hearing loss as a result of cochlear oxidative stress and homocysteine accumulation.80 Other preclinical and observational data implicate high homocysteine levels in hearing loss and cochlear dysfunction.81,82
Vitamin D
Multiple observational studies have found an association between vitamin D deficiency and hearing loss. An observational study in over 1,100 Americans over age 70 found vitamin D deficiency (<20 ng/mL) was associated with hearing loss.83 Another such study that included 3,489 individuals over age 50 found vitamin D deficiency was correlated generally with hearing impairment and specifically with sensorineural hearing loss.84 In observational studies that analyzed data from subjects with type 2 diabetes, low vitamin D levels were associated with a higher risk of hearing loss.85,86 Even in the absence of hearing loss, adequate serum vitamin D appeared to be protective of cochlear health in another observational study.87
Omega-3 Fatty Acids
A study that used data from 65,215 women in the Nurses’ Health Study II found higher intake of omega-3 fatty acids from fish was correlated with a lower risk of developing hearing loss during about 18 years of monitoring. In fact, those who ate two to four fish servings per week were 20% less likely to develop hearing loss compared with those who ate fish less than once a month.88 Another study examined the relationship between omega-3 fatty acid intake and age-related hearing loss in 2,956 subjects aged 50 years and older. The study found higher omega-3 fatty acid intake was associated with a lower likelihood of having age-related hearing loss upon enrollment, and was linked to lower odds of developing age-related hearing loss during about five years of follow-up.89 Findings from animal research also suggested omega-3 fatty acids may protect against progression of hearing loss and improve cochlear metabolism, possibly by suppressing inflammation and homocysteine-related genes.90
Carnitine
The non-essential amino acid carnitine plays a vital role in mitochondrial function and cellular metabolism. Carnitine and its derivative acetyl-L-carnitine have been examined in preclinical research for their potential benefits in age-related health problems, including neurological disorders such as Alzheimer and Parkinson diseases.91,92 Animal studies have suggested L-carnitine supplementation may protect against drug-induced ototoxicity,93 and acetyl-L-carnitine may reduce noise-induced damage to hair cells.94 However, studies examining their possible preventive effect against age-related hearing loss have yielded mixed results.95-97
Melatonin
Melatonin is a hormone that regulates circadian rhythms in the body and has antioxidant and anti-aging properties. An observational study in 126 healthy older adults found lower melatonin levels were associated with increased difficulty hearing high-pitched sounds.98 In animal research, melatonin supplementation has been found to reduce age-related,99,100 noise-induced,101,102 and ototoxic103 hearing loss, as well as hearing loss due to radiation therapy.104 In a laboratory study, melatonin reduced oxidative stress, inflammation, and abnormal protein production in hair cells exposed to nicotine, suggesting it may have a role in decreasing cigarette smoke-induced hearing loss.105
Ginseng
Ginseng (Panax species) is a family of related plants that have been used in traditional herbal medicine systems for centuries to build stress resilience and slow the progression of age-related health problems.106,107 Studies in animal models indicate ginseng may delay age-related hearing loss108 and protect against noise-induced hearing changes109,110 and ototoxicity.111,112 In addition, a laboratory study found ginseng extract prevented drug-induced ototoxic injury in cochlear cells.113 In a randomized controlled trial with 48 textile workers exposed to occupational noise, 14 days of treatment with 200 mg ginseng extract daily resulted in reduced noise-related temporary hearing loss.25 However, in a controlled trial in 73 patients with sudden sensorineural hearing loss, the addition of Korean red ginseng (Panax ginseng), at a dose of 3 grams daily for 20 days, to standard oral corticosteroid therapy did not lead to greater therapeutic effects.114
4 Dietary & Lifestyle Considerations
Hearing loss was long assumed to be an inevitable consequence of aging. However, there is increasing evidence that hearing loss can be prevented or delayed, as well as treated.
Use Hearing Protection and Lower the Volume
Because noise-induced hearing loss is a common and preventable form of acquired hearing loss, the best prevention methods include—if possible—avoiding loud noises, moving away from loud sound sources, taking breaks from noise exposure if it cannot be completely avoided, and turning the volume down.115,116 In addition, using physical ear protection during noise exposure can help preserve hearing.117,118 Unfortunately, a 2021 study from the National Institute for Occupational Safety and Health found that more than half of all noise-exposed workers did not usually use such protection while on the job.119
There are two main types of occupational hearing protection devices: earmuffs that cover the outer ear, and ear plugs or canal caps that block only the ear canal. It is most important that a chosen device provides adequate protection for the type of noise exposure. Look for noise reduction ratings, which indicate the degree (or decibels [dB]) of protection, and check for comfort, convenience, and any other feature that could enhance their likelihood of being used.115,120
Occupational hearing protection devices generally offer a passive approach to noise reduction by simply blocking noise. On the other hand, "noise cancelling” headphone technology is an active, microphone-based approach to noise reduction typically used in recreational listening devices such as headphones and earbuds. The potential benefit of noise-cancelling technology on hearing preservation when listening to music in noisy environments is still under investigation.121 Whether or not noise cancelling technology is used, limiting high-volume recreational noise exposure by reducing the volume on listening devices and using hearing protection at music venues such as nightclubs and concerts are important ways to preserve hearing over time.122
Eat a Healthy Diet
Research has shed light on multiple dietary factors with relationships to hearing loss and its risk factors (eg, chronic inflammation and obesity).123,124
Observational evidence has indicated low or deficient intake of a number of micronutrients may contribute to hearing loss. These include vitamins A, B, C, D and E, and the minerals zinc, magnesium, selenium, iron, and iodine. In addition, higher carbohydrate, fat, and cholesterol intake, and lower protein consumption, have been associated with increased hearing loss risk.125 An observational study that followed 105,592 individuals at least 40 years of age for a median of 3.2 years found higher intake of polyunsaturated fat, particularly in place of saturated fat, was correlated with lower risk of developing disabling hearing impairment.126 In an observational study with 2,956 participants aged 50 years and older, those with a higher intake of cholesterol were more likely to have age-related hearing loss, whereas higher monounsaturated fat intake was linked to a lower chance of this condition.127
A large, questionnaire-based, observational study that included data from 34,576 subjects between 40 and 69 years of age upon enrollment found that those who ate diets high in vitamin D, fruits and vegetables, and protein had lower odds of reporting hearing difficulty, while those who ate high-fat diets were more likely to report hearing problems.128 Another large observational study in nearly 6,000 Korean subjects found that the highest level of dietary potassium intake was associated with the lowest prevalence of hearing loss.129 Plant foods, including most fruits and vegetables, are rich in potassium. High potassium intake in this study may have been a marker for a healthy diet with an abundance of plant foods.
Maintain a Healthy Weight and Metabolism
Maintaining a healthy weight serves as a protective factor against hearing loss. In recent data from the National Health and Nutrition Examination Surveys, obesity was associated with an increased risk of hearing loss.130 A study in over 94,000 individuals, the majority of whom were from Korean populations, found that having more components of metabolic syndrome increased the chances of hearing loss. Metabolic syndrome is a cluster of conditions related to cardiovascular disease and type 2 diabetes risk, comprising abdominal obesity, elevated blood sugar and triglyceride levels, high blood pressure, and low HDL-cholesterol level.131 Another observational study in over 48,000 individuals aged 20 to 64 years noted that obese individuals with metabolic syndrome were 26% and 48% more likely to develop low-frequency and high-frequency hearing loss, respectively, compared with healthy individuals during about seven years of monitoring.132 In one study in South Africa, 106 subjects with hypertension and 92 matched subjects with normal blood pressure underwent audiometric testing; 37.4% of those with hypertension were found to have hearing deficits, while only 14.1% of those without hypertension had hearing deficits.133 Physical activity is also a factor in maintaining a healthy body weight and metabolism, and possibly staving off hearing loss. A study in 2,490 U.S. adults found a correlation between lower physical activity level and worse hearing.134
Stop Smoking
Smoking is well known to contribute to many of the deadliest and most debilitating chronic degenerative diseases, including cancer and cardiovascular disease. It has also been shown to be a risk factor for hearing loss. In an observational study of 3,414 participants aged 72 to 94 years who were followed for roughly 30 years, those who actively smoked had worse results on hearing tests. Interestingly, in those who quit smoking during the study, audiometric outcomes were similar to those of non-smokers and former smokers, suggesting that smoking cessation could be a valuable intervention against hearing loss.135 Another study has shown that tobacco smokers had greater odds of high-frequency hearing loss compared to non-smokers; however, this risk did not extend to cannabis users.136 E-cigarettes, which are growing in popularity, may also have negative impacts on hearing. Findings from a preclinical study suggest non-nicotine components of e-cigarettes have damaging effects on middle ear cells.137 For reasons that are currently not well understood, e-cigarettes have also been linked to sudden hearing loss.138
5 Hearing Loss Causes and Risk Factors
Advancing age and noise exposure are two of the most common risk factors for hearing loss. Infections, earwax impaction, autoimmune disease, and drug reactions also account for a substantial share of hearing loss cases.15 Trauma and tumors can also cause hearing loss, and genetic disorders are important causes of deafness in children.139 In addition to the causes and risk factors discussed in this section, there are a variety of other less common causes of hearing loss.
Age
Age-related hearing loss, or presbycusis, is typically bilateral (affecting both ears), progressive, and irreversible. It is characterized by reduced hearing sensitivity, especially at higher frequencies, and difficulty understanding speech over background noise. For example, having a conversation at a dinner table at a loud restaurant is frequently challenging for a person with age-related hearing loss. In addition to age and genetics, cumulative noise exposure, smoking, and medications can all contribute to age-related hearing loss.140
The aging cochlea displays several features that may contribute to hearing loss, including structural changes to blood vessels and nerves.141 In addition, sensory hair cell loss, degenerative changes in the cochlear nerve (also known as the auditory or acoustic nerve), and other structural changes appear to be involved.140 More recently, it has been hypothesized that chronic low-grade inflammation, sometimes referred to as “inflammaging,” may play a role in age-related hearing loss as it does in other chronic progressive conditions of aging. Inflammaging can be stimulated by a range of factors, including disordered gut microbiota, which can create a pro-inflammatory environment in the digestive tract and promote systemic inflammation.142
Noise Exposure
Exposure to prolonged or extremely loud sounds from sources such as occupational noise, recreational activities, or firearms has been strongly correlated with an increased risk of unilateral (one-sided), bilateral (two-sided), and high-frequency hearing loss.146 An estimated 10‒40 million adults and more than 5 million children are affected by irreversible hearing loss due to excessive noise exposure.117,147,148
It is estimated that as many as 100 million Americans are chronically exposed to sound levels known to be hazardous to auditory function,148 including approximately 22 million U.S. workers exposed to loud noise levels at work.149 The World Health Organization has advised that exposure to sounds at or exceeding 70 dB for 24 hours or 85 dB for one hour can result in hearing impairment and should be avoided.150 Gas-powered leaf blowers, lawn mowers, and city traffic (from inside a car) generate a noise level of 80–85 dB. Longer duration exposure to these noise levels is more harmful because it does not allow the ears time to rest and recover. Short-term exposure to very loud noises (like fireworks or gunfire) can also induce hearing loss.151
Not only does excessive noise damage hearing, but it may also increase blood pressure and heart rate, increase physiologic stress, and raise cortisol levels.152 Increased noise pollution has also been linked to mental health disorders, high blood pressure, and blood vessel dysfunction.153 Noise can damage cochlear tissues through a variety of mechanisms that are also factors in age-related hearing loss, such as increased inflammation and free radical production, disordered calcium metabolism in the inner ear, altered cell signaling, and programmed cell death, all of which have been implicated in hair cell and auditory neuron damage.154
Infections
Infections account for a large portion of temporary hearing loss in both children and adults. Infections involving the outer or middle ear can cause accumulation of debris, local swelling, and tissue inflammation that block sound waves from reaching the inner ear. Symptoms associated with ear infections include a sensation of fullness or pressure in the ear, ear pain or itching, drainage from the ear, fever, and hearing loss.8,15
Earwax (Cerumen)
Earwax, or cerumen, is naturally produced in the external ear canal and helps moisturize the ear and prevent ear infections by maintaining a natural barrier; however, in some individuals, earwax builds up in the ear canal and causes hearing loss by preventing sound from reaching the auditory organs. Earwax impaction is more likely to occur in individuals who routinely wear hearing aids or ear plugs, as well as those with anatomical abnormalities of the ear canal. It affects up to 6% of the population, including about 10% of children and more than 30% of the elderly.155
Ototoxic Drugs
Some drugs have the potential to cause hearing loss or tinnitus because they are ototoxic (ie, toxic to the ear). Examples of ototoxic drugs include certain antibiotics (eg, erythromycin [Erythrocin], clarithromycin [Biaxin], and azithromycin [Zithromax]), a number of chemotherapy drugs (eg, cisplatin [Platinol], carboplatin [Paraplatin], methotrexate [Otrexup], and vincristine [Oncovin]), loop diuretics (eg, furosemide [Lasix], bumetanide [Bumex], and ethacrynic acid [Edecrin]), acetaminophen (Tylenol), and non-steroidal anti-inflammatory drugs (NSAIDs) (eg, aspirin, ibuprofen [Advil], and naproxen [Aleve]).156-158 A number of factors influence the potential for a drug to be ototoxic, such as dosage and duration of treatment, lifetime dose, kidney function, and simultaneous use of multiple ototoxic medications. Hearing loss or tinnitus that results from high doses of aspirin and related medications is usually temporary.159
6 How is Hearing Loss Assessed and Diagnosed?
Screening for hearing loss is often the first step in the assessment of hearing loss. In cases of sudden, noticeable hearing loss, a hearing test may not be necessary. However, a great deal of hearing loss is gradual and progresses imperceptibly. This is very often the case for age-related hearing loss, and elderly individuals may not realize their hearing has diminished, or they may dismiss it as a normal part of aging. Hearing loss in young children can also be overlooked.15,160
A general and hearing-specific medical history can provide diagnostic clues by revealing symptoms, events, conditions, and medications that may be related to hearing loss. In addition, smoking, family history of hearing loss, history of occupational or other loud noise exposure, and other potential contributing factors should be discussed.15,160 In some cases, blood tests such as blood glucose and thyroid hormone levels may be ordered.
Otoscopic examination of the ear canal and ear drum can reveal middle ear causes of hearing loss (eg, cerumen impaction, middle ear infection, or perforated ear drum). A physical exam for hearing loss may also include a “whisper test” to assess hearing ability, as well as detect one-sided hearing loss. Tuning fork testing is another part of a physical exam to assess hearing. The two parts of the tuning fork exam are the Weber and Rinne test. The Weber test helps identify one-sided hearing loss while the Rinne test compares sound transmission through the air versus through the bones of the skull. These tests can suggest whether hearing loss is conductive or sensorineural.15,160
Audiologic testing, performed by an audiologist in a soundproof booth or room, should be performed when the nature of hearing loss is not clear. For instance, this step will often not be necessary when a possible cause such as cerumen impaction or middle ear infection is present. Audiologic testing may include several different components, such as:
- Audiogram. An audiogram (also known as pure tone audiometry) identifies the lowest threshold at which sounds of various frequencies are detected.161 Hearing thresholds are measured in decibels (dB), and sound frequencies, or pitches, are measured in hertz (Hz). Decibels are on a logarithmic scale, such that an individual with a hearing threshold of 30 dB at 1,000 Hz has 10 times poorer hearing than an individual with a hearing threshold of 20 dB, and 100 times poorer hearing than an individual with a threshold of 10 dB.162
- Speech audiometry. Speech audiometry includes two components: the speech reception threshold and the word recognition score. Speech reception is the softest intensity for which the patient can correctly repeat 50% of spoken words. The test is often performed using common two-syllable words. The word recognition score is the percentage of words that are correctly identified when presented at a sound level that is audible to the patient. The word recognition score can help determine whether hearing aids are likely to be beneficial, and it can also help locate the exact site of the hearing problem.8,15
- Tympanometry and acoustic reflex. Tympanometry is used to further characterize hearing loss. The test is performed using a tympanometer (ear plug device) that is placed in the ear canal. By generating various pressure changes and tones, the tympanometer can determine if there is an ear drum perforation, fluid in the middle ear, negative pressure buildup, or abnormal stiffness of the ear drum. Tympanometry can ultimately help assess the cause and type of hearing loss in an individual.163
Additional audiologic and neurologic testing may also be indicated.8,15
7 Treatment of Hearing Loss
The treatment of hearing loss depends on its cause. There are numerous devices as well as medical and surgical therapies available for the treatment of conductive, sensorineural, and mixed hearing loss. This section details some of the most common and important treatment options available.
Devices
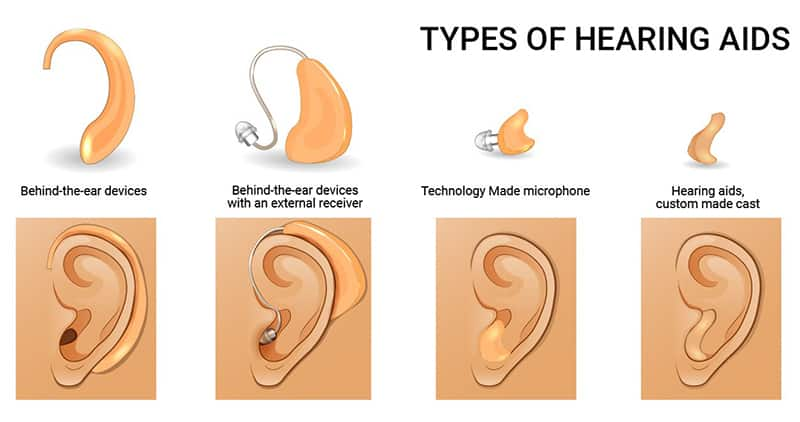
Hearing aids. Conventional hearing aids (ie, small electronic devices worn in or behind the ear) are among the most used treatments for hearing loss. It is estimated that nearly 29 million American adults could benefit from using hearing aids. Hearing aids have three basic parts: microphone, amplifier, and receiver (speaker). The hearing aid receives sound through the microphone, amplifies the sound, and sends it through the ear canal to be transmitted via the auditory system.164
There are several different types of hearing aids to meet the needs of individuals with different preferences, anatomy, and severity of hearing loss.165 Behind-the-ear hearing aids are appropriate for mild-to-profound hearing loss. They are easily visible, which may be a disadvantage to some people; however, they are also easy to handle and typically last a long time. Receiver-in-canal hearing aids are similar but generally smaller and less visible than behind-the-ear aids. They leave the ear canal more open than other types of hearing aids, and therefore may be preferable to those prone to excess earwax and those who experience a plugged sensation when using other types of hearing aids. In-the-ear hearing aids are appropriate for mild-to-severe hearing loss, and they sit completely in the “bowl” where the outer ear meets the ear canal. These devices are custom fitted to the user’s ear shape. In-the-canal and completely-in-the-canal hearing aids are the smallest and least visible devices, but they are only appropriate for mild-to-moderate hearing loss. Due to their small size, patients may find it difficult to manipulate the tiny controls on these devices.165-167
Additional features may be available, such as rechargeable batteries and volume adjustment.165-167
Assistive listening devices. Assistive listening devices or systems are different from hearing aids. They function as a type of amplifier than can aid in one-on-one communication or help in group settings (eg, classrooms or theaters). For example, directional microphones that focus on sound from a certain direction can help improve speech understanding in noisy backgrounds. Another option is a telecoil that can be installed in hearing aids or cochlear implants. A telecoil can allow the device’s electronic circuitry to pick up sound directly from compatible phones or sound systems in public places, such as theaters, classrooms, or houses of worship.172
There are five general types of assistive hearing devices: audio induction (hearing loop), FM system, infrared system, personal amplified system, and Bluetooth system. They are meant to separate the sound a person wants to hear, often voices or speech, from background noise. Assistive listening devices can be used along with hearing aids and cochlear implants, and they can help all levels of hearing loss.173-175
Cochlear implants. Patients with severe-to-profound sensorineural hearing loss may be candidates for cochlear implants. Cochlear implants are devices that convert sound waves into electrical signals that can directly stimulate nerves in the cochlea. It is a valuable option in certain cases of severe-to-profound sensorineural hearing loss.176 Cochlear implantation in older adults has been demonstrated to improve speech recognition, quality of life, and autonomy. Increasing evidence suggests cochlear implants may also improve cognition.177,178 In contrast to hearing aids, cochlear implants are covered by many insurance companies.179
| Table 1: Devices for Treating Hearing Loss | ||||
|---|---|---|---|---|
| Device Category | Description | Indications | Advantages | Disadvantages |
| Hearing Aids166,180 |
Wearable in or behind the ears Amplify ambient sounds to audible levels |
Mild-to-profound hearing loss, depending on the hearing aid type, in children and adults |
A wide range of types, features, and prices Over-the-counter hearing aids are available to adults with mild-to-moderate hearing loss |
Larger behind-the-ear types are highly visible Smaller types may be hard to handle May not be helpful in noisy environments due to lack of sound discrimination |
| Assistive Listening Devices172,181 |
Amplify specific sounds the wearer wants to hear |
Any degree of hearing loss |
Can be used with hearing aids or cochlear implants Allow for amplification of a specific sound or voice in the context of a noisy environment Can be paired with a sound source device such as a telephone, television, microphone, public address system, or other audio system |
May be expensive Various technologies and configurations available, some of which can be complex Additional device to manage |
| Cochlear Implants177-179 |
Convert sound waves into electrical impulses that stimulate nerves in the auditory system |
Severe-to-profound sensorineural hearing loss |
Frequently covered by insurance Not visible outside the ear May improve speech recognition, quality of life, autonomy, and cognition in older individuals |
Require surgery for placement |
Procedures & Medical Treatments
Earwax impaction removal. Earwax (cerumen) impaction is one of the most common, and probably most treatable, acute causes of conductive hearing loss worldwide. Some causes of earwax impaction include hair in the external auditory canal, increasing age, and use of cotton swabs.182
Earwax can be removed by irrigation, manual extraction, cerumenolytic agents such as hydrogen peroxide, or a combination of methods. Physicians in the emergency room and urgent care may elect to remove cerumen using irrigation, as it requires minimal training.183 However, irrigation does carry a small risk of ear canal infection and even tympanic membrane perforation. In cases of unsuccessful earwax removal, or resulting complications, a referral to a qualified Ear, Nose, and Throat (ENT) physician (an otolaryngologist) is made.184
Treating ear infections. External, middle, or inner ear infections can cause acute hearing loss. External and middle ear infections are diagnosed using symptom history, physical exam, and otoscopy (ie, procedure examining the inner structures of the ear). Treatment depends on the site of infection and suspected infectious organism. Most research on middle ear infections has been conducted in children.187,188 Labyrinthitis (an inner ear infection) can result in hearing loss as well as vertigo, nausea and vomiting, and tinnitus. Labyrinthitis often develops following a viral infection, but can be bacterial or the result of an autoimmune disease. Treatment usually involves rest, as well as medications with anti-vertigo effects (eg, meclizine [Dramamine Less Drowsy] or lorazepam [Ativan]) if needed for symptom relief, and high-dose steroids to reduce inflammation in severe cases.189
Treating otosclerosis. Otosclerosis is a progressive disease that results in abnormal bone remodeling in the middle and inner ear, disrupting the transmission of sound from the external ear to the brain. Fixation of the stapes (the third hearing bone) is the most common manifestation of otosclerosis. When stapes fixation occurs, the stapes is unable to vibrate and transmit sound. Possible causes of otosclerosis include previous infections, genetics, and autoimmunity.190
Currently, surgical replacement of the stapes with a prosthetic implant remains the best possible treatment option.191 Treatment with sodium fluoride and bisphosphonates have been considered, but have demonstrated little to no benefit.192 Abnormalities of other hearing bones may also present, and treatment with other prosthetic implants may help recreate natural hearing.193 Bone cement may also be used to refashion the hearing bones.194
8 Novel and Emerging Hearing Loss Treatment Approaches
There is ample research being conducted on preventing and treating hearing loss. Areas of active investigation include gene and stem cell therapy, biomaterials and tissue engineering, novel drug delivery systems, the role of chronic diseases (eg, autoimmune diseases), influence of noise exposure, and importance of biochemical signaling pathways affecting the inner ear, particularly cochlear hair cells.20,195-198
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT), a treatment that has uses for a variety of clinical conditions (eg, radiation damage, crush injuries, skin grafts, and burns),199 in conjunction with other therapies has been shown to reduce the severity of sudden sensorineural hearing loss.200 HBOT involves breathing pure oxygen, generally at a level of atmospheric pressure 1.5–3 times higher than sea level, in a specially designed chamber. In this environment, the lungs can gather significantly more oxygen which could provide antimicrobial, immunomodulatory, and angiogenic effects. Typical sessions last 1.5–2 hours and are repeated from 20 to 60 times, depending on the clinical condition.199,201
Decreased oxygenation in the cochlea may be a potential cause of sudden sensorineural hearing loss. It has therefore been hypothesized that HBOT, which increases oxygenation of the tissues in the cochlea, can assist with sudden sensorineural hearing loss. A meta-analysis published in 2022 assessed randomized controlled trials evaluating HBOT against control therapies (steroids and/or placebo) in participants with sudden sensorineural hearing loss. The combined trials included 88 participants who received HBOT and 62 control participants. The HBOT group had a mean hearing gain of 10.3 dB and 4.3 times greater odds of hearing recovery compared with the control group.200
In a randomized controlled trial published after the meta-analysis, a total of 171 patients with sudden sensorineural hearing loss were enrolled to receive HBOT, oral steroids, or a combination of both therapies. Patients were evaluated by an audiometry test at baseline and again 20 days after treatment. The HBOT treatment encompassed daily sessions from Monday through Friday at 2.5 atmospheric pressure with 90 minutes per session for a total of 10 sessions. The steroid treatment was oral prednisone, 1 mg/kg daily (max dose 60 mg daily), for 12–14 consecutive days. For those who began treatment within seven days after sudden sensorineural hearing loss onset, HBOT alone resulted in the greatest improvements; however, for those beginning treatment later, the combination therapy worked better. Combination treatment and HBOT alone were equally effective in those with profound sensorineural hearing loss (meaning thresholds of 90 dB or more in each test frequency).202
Statins
Statins are a class of cholesterol-lowering medications that includes such widely prescribed drugs as atorvastatin (Lipitor), lovastatin (Mevacor), and rosuvastatin (Crestor). Statins have been found to lower oxidative stress and inflammation, leading to interest in their potential health-promoting and anti-aging effects, including their possible benefits in hearing loss.203
An observational study that included 2,956 participants aged 50 years and older found statin use was correlated with lower prevalence of age-related hearing loss. The study also found an association between higher dietary cholesterol intake and higher odds of age-related hearing loss.127 In an observational study in 84 subjects who had hearing tests before and after starting a statin medication for high cholesterol levels, hearing sensitivity at 6,000 Hz increased and tinnitus severity decreased after treatment.204 However, in a pilot trial, 13 months of treatment with atorvastatin was no better than placebo for improving hearing function in 50 patients with age-related hearing loss and moderately high cholesterol levels.205
An observational study that examined data from 4,387 Korean men and women aged 40 years and older with hearing impairment and 17,548 matched individuals with normal hearing found that among men and individuals aged 70 years and older, those with hearing impairment were less likely to have used statins in the previous two years.206 Other observational studies have linked statin use with a slightly lower risk of sudden sensorineural hearing loss,207 lower risk of sensorineural hearing loss in type 2 diabetics,208 and lower risk of ototoxicity in cancer patients treated with the chemotherapy drug cisplatin.209
Ebselen
Ebselen, a synthetic molecule with antioxidant, anti-inflammatory, and neuroprotective properties, has been studied as a treatment option for noise-induced hearing loss.210 In a randomized, double-blind, placebo-controlled trial that included 81 healthy subjects, those who received 400 mg ebselen twice daily for four days, beginning two days before testing, exhibited 68% less of a temporary decrease in hearing 15 minutes after an experimental loud sound exposure compared with placebo.211 STOPMD-3, a late-stage clinical trial investigating the efficacy of ebselen in the treatment of hearing loss and tinnitus in Ménière disease, is in progress as of May 2023.212
Gene and Stem Cell Therapies
Genetic factors play a role in about one-half of all cases of sensorineural hearing loss, but treatments to address genetic causes are generally not available. Two gene therapies that have been investigated are gene replacement, which is intended to replace non-functional DNA in cells with properly functioning DNA, and gene silencing, which attempts to prevent transcription of relevant gene mutations. A newer gene therapy that holds promise for the treatment of hearing loss is CRISPR/Cas9-based genome-editing, in which segments of DNA are added, removed, or altered. In an animal model of hearing loss, the use of CRISPR/Cas9 technology resulted in increased hair cell survival.20
Another promising area of research is stem cell therapy. Stem cell therapy, either alone or in combination with gene therapies, may help restore healthy nerve tissue in the auditory network.213,214 For instance, pluripotent stem cells (which have the ability to generate multiple types of functional cells) have been used to produce hair cells, ear sensory neurons, and cochlear nerve cell bodies.215
Eventually, gene and stem cell therapies could help address both genetic causes of hearing loss as well as more common sensorineural hearing loss. For now, readily available solutions such as hearing aids, assistive listening devices, and cochlear implants are more viable treatment options.196
Biologic Immune-Modulating Agents
Biologic agents have been studied in certain types of autoimmune hearing loss. Autoimmune hearing loss is caused by an immune dysfunction in which hearing and balance organs are mistaken as foreign tissues and attacked by antibodies, triggering inflammatory processes. This type of hearing loss can accompany autoimmune conditions such as Cogan syndrome, systemic lupus erythematosus, rheumatoid arthritis, and inflammatory bowel disease. Therapies involving engineered antibodies that target specific molecules in the immune system may help by disrupting the autoimmune process. Infliximab (Remicade), which targets the cytokine tumor necrosis factor [TNF]-α), and rituximab (Rituxan), which targets a protein on certain immune cells, have been shown to reduce the number of inflammatory cells in the cochlea and thereby stabilize hearing in patients with autoimmune hearing loss.216 Interestingly, an antibody targeting anti-intercellular adhesion molecule-1 has been studied in the context of noise-induced hearing loss. In a controlled animal study, treatment with this antibody reduced the degree of noise-induced temporary hearing impairment.217 In the future, direct delivery of pharmacologic agents to the inner ear may open up new treatment options.218,219
9 The Consequences of Untreated Hearing Loss
The ability to convert mechanical sound waves into electrical signals that travel to and are interpreted in the brain is a vital function, and hearing loss can lead to several important neurological changes. Specifically, people with long-term hearing loss have been found to have increased gray matter atrophy (shrinkage) in certain brain regions compared to those without hearing loss.220 Age-related hearing loss in the elderly has been associated with cognitive impairment and dementia. In one study of nearly 38,000 elderly men who were dementia-free at the beginning of the study, those with hearing loss had a 69% higher risk of developing dementia during an average of 11.1 years of follow-up.221 Hearing loss has also been correlated with earlier onset of cognitive decline.222
There are multiple theories that attempt to explain the link between hearing loss and dementia. Some are mechanistic and relate to structural and biochemical factors in brain function. For example, one mechanistic theory to explain the association postulates that chronic loud noise exposure (a risk factor for hearing loss) leads to a toxic microenvironment in the brain’s hippocampus. This toxicity is characterized by elevated levels of markers of oxidative stress and neurotoxicity, as well as spikes in glucocorticoid levels. This leads to interrupted nerve cell formation (neurogenesis), loss of neural connections, and accumulation of a neurotoxic protein called hyperphosphorylated tau in the hippocampus. Hippocampal structural damage and dysfunction are considered hallmarks of Alzheimer disease.223
Age-related hearing loss is accompanied by other age-related neurological changes and may result in social isolation, both of which could contribute to cognitive decline. Another theory linking hearing loss to cognitive dysfunction suggests decreased hearing leads to a strain on cognitive resources generally.224
Although a causal link between hearing loss and dementia or Alzheimer disease has yet to be conclusively established, there is relative consensus that age-related hearing loss is closely associated with cognitive impairment, cognitive decline, and dementia.225-227 Importantly, age-related hearing loss has been identified as one of the most modifiable risk factors for dementia.228
From a psychological standpoint, hearing loss is associated with depression, anxiety, and social isolation.229 A meta-analysis of 35 observational studies found that older adults with hearing loss had 47% greater odds of depression.230 Subsequent studies continue to confirm that hearing loss is strongly correlated with depression and other neuropsychiatric symptoms.231,232 This may be due in large part to impairments in communication and a reduction in activities of daily living. Furthermore, individuals with hearing loss have been shown to be unlikely to seek help.229 On the other hand, engagement in mentally stimulating activities has been shown to reduce depression symptoms in those with hearing loss.233
Bilateral hearing loss was found to be associated with high blood pressure in occupational noise-exposed workers. This risk was higher in those with prolonged exposure, as well as in males.234 Hearing loss is also a risk factor for falls and car accidents in the elderly.235 In one observational study, poor hearing was associated with more variable stride length, which was correlated with increased risk of falling.236 Falls, especially in the elderly population, can have devastating effects on overall health and quality of life, and can even result in death. Hearing loss has also been linked with reduced job performance, tension, stress, and reduced alertness.237
In children, hearing loss can cause detrimental effects on speech, language, and developmental and cognitive outcomes.238 Children with hearing loss are at risk for delays in cognitive function.239 In a study involving over 22,000 Danish young men, even mild hearing loss was associated with a reduced likelihood of continuing education beyond age 16, and the likelihood was lower still among those with severe hearing loss.240 There is also a link between hearing loss and various behavioral and emotional problems.241
10 Hearing Loss: Frequently Ask Questions
Do headphones cause hearing loss?
Headphones are not necessarily a threat to hearing, but chronic exposure to loud noise of any kind is a known risk factor for developing hearing loss later in life. It is estimated that 50% of individuals who use headphones are listening at volumes that can cause long-term hearing loss.242
Is there a relationship between hearing loss and dementia?
Hearing loss is a risk factor for cognitive decline and dementia, but the relationship has not been proven to be causal. Treating hearing loss may improve both quality of life and cognition.178,243
Is hearing loss a disability?
Profound hearing loss is considered a disability.244 The World Health Organization defines disabling hearing loss as a loss of 35 dB or more in the less affected ear.245
Does listening to white noise cause hearing loss?
White noise, like any noise, can be harmful to hearing if it is too loud. Tests of white noise machines intended for infants and babies showed they can exceed recommended safe noise exposure levels. White noise machines should therefore be used at a low volume setting and placed away from the ear.246
How many decibels could cause hearing loss?
The louder the sound, the shorter the safe listening time. For instance, a sound level of 75 dB (such as from a vacuum cleaner) is considered unsafe after eight hours, whereas a sound level of 80 dB is unsafe after two hours, and 85 dB is unsafe after one hour (for context, gas-powered lawn mowers and leaf blowers produce about 80–85 dB). Listening to music at the maximum setting on many personal listening devices, which reach 105–110 dB, can cause hearing loss in just five minutes.151
Who is at risk for hearing loss?
Older individuals, people who are regularly exposed to loud noise at work or recreationally, patients taking drugs that have toxic effects on the ears, those who have had recurrent ear infections, people prone to earwax impaction, and smokers are among those at risk for hearing loss.247
Can hearing loss happen suddenly?
Sudden sensorineural hearing loss is an uncommon condition that may be related to infection, head trauma, autoimmune disease, blood circulation problems, or exposure to certain drugs, but in most cases the cause is unknown.248
Can hearing loss be reversed?
In many cases hearing loss is irreversible, but when caused by a treatable or temporary condition, like cerumen impaction or acute infection, hearing can usually be fully recovered.15
Does hearing loss cause tinnitus?
Hearing loss is the most common cause of tinnitus, and the two conditions share certain risk factors, such as older age and noise exposure. Tinnitus is often the first sign of hearing loss in older individuals, and hearing loss treatment can sometimes improve tinnitus.249
How does hearing loss affect the brain?
A close relationship between hearing loss and cognitive disorders has been identified.226 Although it is still unclear whether hearing loss is the cause of changes in brain structure and function, intriguing evidence has shown individuals with prolonged hearing loss experience shrinkage of certain brain regions.224
Is hearing loss hereditary?
The majority of hearing loss and deafness seen in babies and young children is hereditary, but genetics generally have only a small role in determining susceptibility to hearing loss in adulthood.250,251
Which hearing aid is best for severe hearing loss?
The choice for type of hearing aid to be used is often dependent on individual preference. For those with severe or profound hearing loss, high-powered hearing aids may provide greater benefit but tend to be more visible.165
Disclaimer and Safety Information
This information (and any accompanying material) is not intended to replace the attention or advice of a physician or other qualified health care professional. Anyone who wishes to embark on any dietary, drug, exercise, or other lifestyle change intended to prevent or treat a specific disease or condition should first consult with and seek clearance from a physician or other qualified health care professional. Pregnant women in particular should seek the advice of a physician before using any protocol listed on this website. The protocols described on this website are for adults only, unless otherwise specified. Product labels may contain important safety information and the most recent product information provided by the product manufacturers should be carefully reviewed prior to use to verify the dose, administration, and contraindications. National, state, and local laws may vary regarding the use and application of many of the therapies discussed. The reader assumes the risk of any injuries. The authors and publishers, their affiliates and assigns are not liable for any injury and/or damage to persons arising from this protocol and expressly disclaim responsibility for any adverse effects resulting from the use of the information contained herein.
The protocols raise many issues that are subject to change as new data emerge. None of our suggested protocol regimens can guarantee health benefits. Life Extension has not performed independent verification of the data contained in the referenced materials, and expressly disclaims responsibility for any error in the literature.
- Madans JH, Weeks JD, Elgaddal N. Centers for Disease Control and Prevention. Hearing Difficulties Among Adults: United States, 2019. Updated 7/28/2021. Accessed 10/3/2022, https://www.cdc.gov/nchs/products/databriefs/db414.htm
- Goman AM, Lin FR. Prevalence of Hearing Loss by Severity in the United States. Am J Public Health. Oct 2016;106(10):1820-2. doi:10.2105/AJPH.2016.303299. https://www.ncbi.nlm.nih.gov/pubmed/27552261
- Dillard LK, Arunda MO, Lopez-Perez L, Martinez RX, Jimenez L, Chadha S. Prevalence and global estimates of unsafe listening practices in adolescents and young adults: a systematic review and meta-analysis. BMJ Glob Health . Nov 2022;7(11)doi:10.1136/bmjgh-2022-010501. https://www.ncbi.nlm.nih.gov/pubmed/36379592
- Reed NS, Altan A, Deal JA, et al. Trends in Health Care Costs and Utilization Associated With Untreated Hearing Loss Over 10 Years. JAMA Otolaryngol Head Neck Surg . Jan 1 2019;145(1):27-34. doi:10.1001/jamaoto.2018.2875. https://www.ncbi.nlm.nih.gov/pubmed/30419131
- Types of Hearing Loss. Updated 2022-03-02. https://www.hopkinsmedicine.org/health/conditions-and-diseases/hearing-loss/types-of-hearing-loss
- Stanford Medicine Children's Health. https://www.stanfordchildrens.org/en/topic/default?id=anatomy-and-physiology-of-the-ear-90-P02025
- VEDA. Ear Anatomy. Accessed 10/25/2022, https://vestibular.org/article/what-is-vestibular/the-human-balance-system/ear-anatomy/
- Weber PC. Etiology of hearing loss in adults - UpToDate. https://www.uptodate.com/contents/etiology-of-hearing-loss-in-adults
- Tanna RJ, Lin JW, De Jesus O. Sensorineural Hearing Loss. StatPearls. StatPearls Publishing Copyright© 2022, StatPearls Publishing LLC.; 2022. https://www.ncbi.nlm.nih.gov/pubmed/33351419
- Blevins NH. Presbycusis. UpToDate. Updated 4/18/2022. Accessed 10/25/2022, https://www.uptodate.com/contents/presbycusis
- Rabinowitz PM. Noise-induced hearing loss. Am Fam Physician. May 1 2000;61(9):2749-56, 2759-60. https://www.ncbi.nlm.nih.gov/pubmed/10821155
- Ganesan P, Schmiedge J, Manchaiah V, Swapna S, Dhandayutham S, Kothandaraman PP. Ototoxicity: A Challenge in Diagnosis and Treatment. J Audiol Otol. Apr 2018;22(2):59-68. doi:10.7874/jao.2017.00360. https://www.ncbi.nlm.nih.gov/pubmed/29471610
- Lustig LR. Meniere Disease. Merck Manual: Professional Version. Updated 9/2022. Accessed 10/25/2022, https://www.merckmanuals.com/professional/ear,-nose,-and-throat-disorders/inner-ear-disorders/meniere-disease
- Koenen L, Andaloro C. Meniere Disease. StatPearls. StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022. https://www.ncbi.nlm.nih.gov/pubmed/30725640
- Lustig LR. Hearing Loss. Merck Manual: Professional Version. Updated 9/2022. https://www.merckmanuals.com/professional/ear,-nose,-and-throat-disorders/hearing-loss/hearing-loss
- Fancello V, Sacchetto L, Bianchini C, Ciorba A, Monzani D, Palma S. Management of Juvenile Otosclerosis: A Systematic Review. Children (Basel) . Nov 21 2022;9(11)doi:10.3390/children9111787. https://www.ncbi.nlm.nih.gov/pubmed/36421236
- Hammill TL, Campbell KC. Protection for medication-induced hearing loss: the state of the science. Int J Audiol. Sep 2018;57(sup4):S67-S75. doi:10.1080/14992027.2018.1455114. https://www.ncbi.nlm.nih.gov/pubmed/29688112
- Gul F, Muderris T, Yalciner G, et al. A comprehensive study of oxidative stress in sudden hearing loss. Eur Arch Otorhinolaryngol. Mar 2017;274(3):1301-1308. doi:10.1007/s00405-016-4301-1. https://www.ncbi.nlm.nih.gov/pubmed/27614879
- Hullfish H, Roldan LP, Hoffer ME. The Use of Antioxidants in the Prevention and Treatment of Noise-Induced Hearing Loss. Otolaryngol Clin North Am . Oct 2022;55(5):983-991. doi:10.1016/j.otc.2022.06.006. https://www.ncbi.nlm.nih.gov/pubmed/36088150
- Ren H, Hu B, Jiang G. Advancements in prevention and intervention of sensorineural hearing loss. Therapeutic advances in chronic disease . 2022;13:20406223221104987. doi:10.1177/20406223221104987. https://www.ncbi.nlm.nih.gov/pubmed/35782345
- Kopke R, Bielefeld E, Liu J, et al. Prevention of impulse noise-induced hearing loss with antioxidants. Acta Otolaryngol. Mar 2005;125(3):235-43. doi:10.1080/00016480410023038. https://www.ncbi.nlm.nih.gov/pubmed/15966690
- Zhitkovich A. N-Acetylcysteine: Antioxidant, Aldehyde Scavenger, and More. Chemical research in toxicology. Jul 15 2019;32(7):1318-1319. doi:10.1021/acs.chemrestox.9b00152. https://www.ncbi.nlm.nih.gov/pubmed/31046246
- Abbasi M, Pourrajab B, Tokhi MO. Protective effects of vitamins/antioxidants on occupational noise-induced hearing loss: A systematic review. J Occup Health . Jan 2021;63(1):e12217. doi:10.1002/1348-9585.12217. https://www.ncbi.nlm.nih.gov/pubmed/33788342
- Kopke R, Slade MD, Jackson R, et al. Efficacy and safety of N-acetylcysteine in prevention of noise induced hearing loss: a randomized clinical trial. Hear Res. May 2015;323:40-50. doi:10.1016/j.heares.2015.01.002. https://www.ncbi.nlm.nih.gov/pubmed/25620313
- Doosti A, Lotfi Y, Moossavi A, Bakhshi E, Talasaz AH, Hoorzad A. Comparison of the effects of N-acetyl-cysteine and ginseng in prevention of noise induced hearing loss in male textile workers. Noise & health. Jul-Aug 2014;16(71):223-7. doi:10.4103/1463-1741.137057. https://www.ncbi.nlm.nih.gov/pubmed/25033789
- Bai X, Chen S, Xu K, et al. N-Acetylcysteine Combined With Dexamethasone Treatment Improves Sudden Sensorineural Hearing Loss and Attenuates Hair Cell Death Caused by ROS Stress. Original Research. Frontiers in cell and developmental biology . 2021-March-18 2021;9:659486. doi:10.3389/fcell.2021.659486. https://www.ncbi.nlm.nih.gov/pubmed/33816510
- Chen SL, Ho CY, Chin SC. Effects of oral N-acetylcysteine combined with oral prednisolone on idiopathic sudden sensorineural hearing loss. Medicine (Baltimore) . Jul 1 2022;101(26):e29792. doi:10.1097/MD.0000000000029792. https://www.ncbi.nlm.nih.gov/pubmed/35777063
- Huang S, Xu A, Sun X, et al. Otoprotective Effects of alpha-lipoic Acid on A/J Mice With Age-related Hearing Loss. Otol Neurotol. Jul 2020;41(6):e648-e654. doi:10.1097/MAO.0000000000002643. https://www.ncbi.nlm.nih.gov/pubmed/32282782
- Han JS, Kim YL, Yu HJ, et al. Safety and Efficacy of Intratympanic Alpha-Lipoic Acid Injection in a Mouse Model of Noise-Induced Hearing Loss. Antioxidants (Basel). Jul 22 2022;11(8)doi:10.3390/antiox11081423. https://www.ncbi.nlm.nih.gov/pubmed/35892625
- Kim J, Cho HJ, Sagong B, et al. Alpha-lipoic acid protects against cisplatin-induced ototoxicity via the regulation of MAPKs and proinflammatory cytokines. Biochem Biophys Res Commun. Jun 27 2014;449(2):183-9. doi:10.1016/j.bbrc.2014.04.118. https://www.ncbi.nlm.nih.gov/pubmed/24796665
- Wang A, Hou N, Bao D, Liu S, Xu T. Mechanism of alpha-lipoic acid in attenuating kanamycin-induced ototoxicity. Neural regeneration research . Dec 15 2012;7(35):2793-800. doi:10.3969/j.issn.1673-5374.2012.35.007. https://www.ncbi.nlm.nih.gov/pubmed/25317129
- Quaranta N, Dicorato A, Matera V, D'Elia A, Quaranta A. The effect of alpha-lipoic acid on temporary threshold shift in humans: a preliminary study. Acta Otorhinolaryngol Ital. Dec 2012;32(6):380-5. https://www.ncbi.nlm.nih.gov/pubmed/23349557
- Takumida M, Anniko M. Radical scavengers for elderly patients with age-related hearing loss. Acta Otolaryngol. Jan 2009;129(1):36-44. doi:10.1080/00016480802008215. https://www.ncbi.nlm.nih.gov/pubmed/18607930
- Rodrigo L, Campos-Asensio C, Rodriguez MA, Crespo I, Olmedillas H. Role of nutrition in the development and prevention of age-related hearing loss: A scoping review. J Formos Med Assoc. Jan 2021;120(1 Pt 1):107-120. doi:10.1016/j.jfma.2020.05.011. https://www.ncbi.nlm.nih.gov/pubmed/32473863
- Alvarado JC, Fuentes-Santamaria V, Melgar-Rojas P, Gabaldon-Ull MC, Cabanes-Sanchis JJ, Juiz JM. Oral Antioxidant Vitamins and Magnesium Limit Noise-Induced Hearing Loss by Promoting Sensory Hair Cell Survival: Role of Antioxidant Enzymes and Apoptosis Genes. Antioxidants (Basel). Nov 25 2020;9(12)doi:10.3390/antiox9121177. https://www.ncbi.nlm.nih.gov/pubmed/33255728
- Gopinath B, Flood VM, McMahon CM, et al. Dietary antioxidant intake is associated with the prevalence but not incidence of age-related hearing loss. J Nutr Health Aging. Dec 2011;15(10):896-900. doi:10.1007/s12603-011-0119-0. https://www.ncbi.nlm.nih.gov/pubmed/22159779
- Choi YH, Miller JM, Tucker KL, Hu H, Park SK. Antioxidant vitamins and magnesium and the risk of hearing loss in the US general population. Am J Clin Nutr . Jan 2014;99(1):148-55. doi:10.3945/ajcn.113.068437. https://www.ncbi.nlm.nih.gov/pubmed/24196403
- Ibrahim I, Zeitouni A, da Silva SD. Effect of Antioxidant Vitamins as Adjuvant Therapy for Sudden Sensorineural Hearing Loss: Systematic Review Study. Audiol Neurootol. 2018;23(1):1-7. doi:10.1159/000486274. https://www.ncbi.nlm.nih.gov/pubmed/29929192
-
Kaya H, Koc AK, Sayin I, et al. Vitamins A, C, and E and selenium in the
treatment of idiopathic sudden sensorineural hearing loss.
Eur Arch Otorhinolaryngol. May 2015;272(5):1119-25. doi:10.1007/s00405-014-2922-9.
https://www.ncbi.nlm.nih.gov/pubmed/24519034
https://link.springer.com/article/10.1007/s00405-014-2922-9 - Kim YR, Baek JI, Kim SH, et al. Therapeutic potential of the mitochondria-targeted antioxidant MitoQ in mitochondrial-ROS induced sensorineural hearing loss caused by Idh2 deficiency. Redox Biol. Jan 2019;20:544-555. doi:10.1016/j.redox.2018.11.013. https://www.ncbi.nlm.nih.gov/pubmed/30508699
- Fetoni AR, De Bartolo P, Eramo SL, et al. Noise-induced hearing loss (NIHL) as a target of oxidative stress-mediated damage: cochlear and cortical responses after an increase in antioxidant defense. J Neurosci. Feb 27 2013;33(9):4011-23. doi:10.1523/JNEUROSCI.2282-12.2013. https://www.ncbi.nlm.nih.gov/pubmed/23447610
- Dirain CO, Ng M, Milne-Davies B, Joseph JK, Antonelli PJ. Evaluation of Mitoquinone for Protecting Against Amikacin-Induced Ototoxicity in Guinea Pigs. Otol Neurotol. Jan 2018;39(1):111-118. doi:10.1097/MAO.0000000000001638. https://www.ncbi.nlm.nih.gov/pubmed/29194212
- Tate AD, Antonelli PJ, Hannabass KR, Dirain CO. Mitochondria-Targeted Antioxidant Mitoquinone Reduces Cisplatin-Induced Ototoxicity in Guinea Pigs. Otolaryngol Head Neck Surg. Mar 2017;156(3):543-548. doi:10.1177/0194599816678381. https://www.ncbi.nlm.nih.gov/pubmed/28248600
- Astolfi L, Simoni E, Valente F, et al. Coenzyme Q10 plus Multivitamin Treatment Prevents Cisplatin Ototoxicity in Rats. PLoS One. 2016;11(9):e0162106. doi:10.1371/journal.pone.0162106. https://www.ncbi.nlm.nih.gov/pubmed/27632426
- Staffa P, Cambi J, Mezzedimi C, Passali D, Bellussi L. Activity of coenzyme Q 10 (Q-Ter multicomposite) on recovery time in noise-induced hearing loss. Noise & health. Sep-Oct 2014;16(72):265-9. doi:10.4103/1463-1741.140499. https://www.ncbi.nlm.nih.gov/pubmed/25209035
- Salami A, Mora R, Dellepiane M, et al. Water-soluble coenzyme Q10 formulation (Q-TER((R))) in the treatment of presbycusis. Acta Otolaryngol . Oct 2010;130(10):1154-62. doi:10.3109/00016481003727590. https://www.ncbi.nlm.nih.gov/pubmed/20443731
- Cadoni G, Scipione S, Agostino S, et al. Coenzyme Q 10 and cardiovascular risk factors in idiopathic sudden sensorineural hearing loss patients. Otol Neurotol. Oct 2007;28(7):878-83. doi:10.1097/MAO.0b013e3180686e4a. https://www.ncbi.nlm.nih.gov/pubmed/17558340
-
Ahn JH, Yoo MH, Lee HJ, Chung JW, Yoon TH. Coenzyme Q10 in combination with
steroid therapy for treatment of sudden sensorineural hearing loss: a
controlled prospective study.
Clinical otolaryngology : official journal of ENT-UK ; official journal
of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial
Surgery. Dec 2010;35(6):486-9. doi:10.1111/j.1749-4486.2010.02201.x.
https://www.ncbi.nlm.nih.gov/pubmed/21199410
https://onlinelibrary.wiley.com/doi/10.1111/j.1749-4486.2010.02201.x - Yeh CW, Tseng LH, Yang CH, Hwang CF. Effects of oral zinc supplementation on patients with noise-induced hearing loss associated tinnitus: A clinical trial. Biomedical journal. Feb 2019;42(1):46-52. doi:10.1016/j.bj.2018.10.009. https://www.ncbi.nlm.nih.gov/pubmed/30987704
- Yang CH, Ko MT, Peng JP, Hwang CF. Zinc in the treatment of idiopathic sudden sensorineural hearing loss. Laryngoscope. Mar 2011;121(3):617-21. doi:10.1002/lary.21291. https://www.ncbi.nlm.nih.gov/pubmed/20928835
- Campbell KC, Rehemtulla A, Sunkara P, Hamstra D, Buhnerkempe M, Ross B. Oral D-methionine protects against cisplatin-induced hearing loss in humans: phase 2 randomized clinical trial in India. Int J Audiol. Aug 2022;61(8):621-631. doi:10.1080/14992027.2021.1983215. https://www.ncbi.nlm.nih.gov/pubmed/34622731
- Campbell KCM, Cosenza N, Meech R, et al. D-methionine administered as late as 36 hours post-noise exposure rescues from permanent threshold shift and dose-dependently increases serum antioxidant levels. Int J Audiol . Feb 2023;62(2):151-158. doi:10.1080/14992027.2021.2022790. https://www.ncbi.nlm.nih.gov/pubmed/35015962
- Wang Y, Qu Y, Chen X, et al. Effects of D-methionine in mice with noise-induced hearing loss mice. J Int Med Res. Aug 2019;47(8):3874-3885. doi:10.1177/0300060519860679. https://www.ncbi.nlm.nih.gov/pubmed/31327277
- Campbell KC, Martin SM, Meech RP, Hargrove TL, Verhulst SJ, Fox DJ. D-methionine (D-met) significantly reduces kanamycin-induced ototoxicity in pigmented guinea pigs. Int J Audiol. 2016;55(5):273-8. doi:10.3109/14992027.2016.1143980. https://www.ncbi.nlm.nih.gov/pubmed/26963517
- Campbell KC, Meech RP, Klemens JJ, et al. Prevention of noise- and drug-induced hearing loss with D-methionine. Hear Res. Apr 2007;226(1-2):92-103. doi:10.1016/j.heares.2006.11.012. https://www.ncbi.nlm.nih.gov/pubmed/17224251
- Costello RB, Nielsen F. Interpreting magnesium status to enhance clinical care: key indicators. Curr Opin Clin Nutr Metab Care. Nov 2017;20(6):504-511. doi:10.1097/MCO.0000000000000410. https://www.ncbi.nlm.nih.gov/pubmed/28806179
- Costello RB, Elin RJ, Rosanoff A, et al. Perspective: The Case for an Evidence-Based Reference Interval for Serum Magnesium: The Time Has Come. Adv Nutr. Nov 2016;7(6):977-993. doi:10.3945/an.116.012765. https://www.ncbi.nlm.nih.gov/pubmed/28140318
- Severino P, Netti L, Mariani MV, et al. Prevention of Cardiovascular Disease: Screening for Magnesium Deficiency. Cardiol Res Pract. 2019;2019:4874921. doi:10.1155/2019/4874921. https://www.ncbi.nlm.nih.gov/pubmed/31192005
- Fang X, Wang K, Han D, et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med. Dec 8 2016;14(1):210. doi:10.1186/s12916-016-0742-z. https://www.ncbi.nlm.nih.gov/pubmed/27927203
- Sendowski I, Holy X, Raffin F, Cazals Y. Magnesium and hearing loss. In: Vink R, Nechifor M, eds. Magnesium in the Central Nervous System. University of Adelaide Press © 2011 The Authors.; 2011. https://www.ncbi.nlm.nih.gov/pubmed/29920019
- Joachims Z, Netzer A, Ising H, et al. Oral magnesium supplementation as prophylaxis for noise-induced hearing loss: results of a double blind field study. Schriftenr Ver Wasser Boden Lufthyg. 1993;88:503-16. https://www.ncbi.nlm.nih.gov/pubmed/8460390
- Attias J, Weisz G, Almog S, et al. Oral magnesium intake reduces permanent hearing loss induced by noise exposure. Am J Otolaryngol. Jan-Feb 1994;15(1):26-32. doi:10.1016/0196-0709(94)90036-1.
- Gordin A, Goldenberg D, Golz A, Netzer A, Joachims HZ. Magnesium: a new therapy for idiopathic sudden sensorineural hearing loss. Otol Neurotol . Jul 2002;23(4):447-51. doi:10.1097/00129492-200207000-00009. https://www.ncbi.nlm.nih.gov/pubmed/12170143
- Scheper V, Schmidtheisler M, Lasch F, et al. Randomized placebo-controlled clinical trial investigating the effect of antioxidants and a vasodilator on overall safety and residual hearing preservation in cochlear implant patients. Trials. Jul 14 2020;21(1):643. doi:10.1186/s13063-020-04522-9. https://www.ncbi.nlm.nih.gov/pubmed/32665006
- Kandiah N, Ong PA, Yuda T, et al. Treatment of dementia and mild cognitive impairment with or without cerebrovascular disease: Expert consensus on the use of Ginkgo biloba extract, EGb 761((R)). CNS neuroscience & therapeutics . Feb 2019;25(2):288-298. doi:10.1111/cns.13095. https://www.ncbi.nlm.nih.gov/pubmed/30648358
- Savaskan E, Mueller H, Hoerr R, von Gunten A, Gauthier S. Treatment effects of Ginkgo biloba extract EGb 761(R) on the spectrum of behavioral and psychological symptoms of dementia: meta-analysis of randomized controlled trials. International psychogeriatrics. Mar 2018;30(3):285-293. doi:10.1017/S1041610217001892. https://www.ncbi.nlm.nih.gov/pubmed/28931444
- Tan MS, Yu JT, Tan CC, et al. Efficacy and adverse effects of ginkgo biloba for cognitive impairment and dementia: a systematic review and meta-analysis. J Alzheimers Dis. 2015;43(2):589-603. doi:10.3233/JAD-140837. https://www.ncbi.nlm.nih.gov/pubmed/25114079
- Si X, Yu Z, Ren X, Huang L, Feng Y. Efficacy and safety of standardized Ginkgo biloba L. leaves extract as an adjuvant therapy for sudden sensorineural hearing loss: A systematic review and meta-analysis. J Ethnopharmacol . Jan 10 2022;282:114587. doi:10.1016/j.jep.2021.114587. https://www.ncbi.nlm.nih.gov/pubmed/34474140
- Sun Y, Xing Y, Jiang X, et al. Effectiveness of Ginkgo biloba diterpene lactone in the treatment of sudden sensorineural hearing loss. Am J Otolaryngol . May-Jun 2021;42(3):102922. doi:10.1016/j.amjoto.2021.102922. https://www.ncbi.nlm.nih.gov/pubmed/33454456
- Achete de Souza G, de Marqui SV, Matias JN, Guiguer EL, Barbalho SM. Effects of Ginkgo biloba on Diseases Related to Oxidative Stress. Planta Med . Apr 2020;86(6):376-386. doi:10.1055/a-1109-3405. https://www.ncbi.nlm.nih.gov/pubmed/32097975
- Tziridis K, Schulze H. Preventive Effects of Ginkgo-Extract EGb 761((R)) on Noise Trauma-Induced Cochlear Synaptopathy. Nutrients. Jul 22 2022;14(15)doi:10.3390/nu14153015. https://www.ncbi.nlm.nih.gov/pubmed/35893868
- Zhu M, Mao M, Lou X. Elevated homocysteine level and prognosis in patients with acute coronary syndrome: a meta-analysis. Biomarkers. Jun 2019;24(4):309-316. doi:10.1080/1354750X.2019.1589577. https://www.ncbi.nlm.nih.gov/pubmed/30821522
- Smith AD, Refsum H. Homocysteine - from disease biomarker to disease prevention. J Intern Med. Oct 2021;290(4):826-854. doi:10.1111/joim.13279. https://www.ncbi.nlm.nih.gov/pubmed/33660358
- Lai WK, Kan MY. Homocysteine-Induced Endothelial Dysfunction. Ann Nutr Metab. 2015;67(1):1-12. doi:10.1159/000437098.
- Esse R, Barroso M, Tavares de Almeida I, Castro R. The Contribution of Homocysteine Metabolism Disruption to Endothelial Dysfunction: State-of-the-Art. Int J Mol Sci. Feb 17 2019;20(4)doi:10.3390/ijms20040867. https://www.ncbi.nlm.nih.gov/pubmed/30781581
- Fasano T, Pertinhez TA, Tribi L, et al. Laboratory assessment of sudden sensorineural hearing loss: A case-control study. Laryngoscope. Oct 2017;127(10):2375-2381. doi:10.1002/lary.26514. https://www.ncbi.nlm.nih.gov/pubmed/28224621
- Fusconi M, Chistolini A, de Virgilio A, et al. Sudden sensorineural hearing loss: a vascular cause? Analysis of prothrombotic risk factors in head and neck. Int J Audiol. Nov 2012;51(11):800-5. doi:10.3109/14992027.2012.705904. https://www.ncbi.nlm.nih.gov/pubmed/22928918
- Quaranta A, Scaringi A, Bartoli R, Margarito MA, Quaranta N. The effects of 'supra-physiological' vitamin B12 administration on temporary threshold shift. Int J Audiol. Mar 2004;43(3):162-5. doi:10.1080/14992020400050022. https://www.ncbi.nlm.nih.gov/pubmed/15198380
- Gopinath B, Flood VM, Rochtchina E, McMahon CM, Mitchell P. Serum homocysteine and folate concentrations are associated with prevalent age-related hearing loss. J Nutr. Aug 2010;140(8):1469-74. doi:10.3945/jn.110.122010. https://www.ncbi.nlm.nih.gov/pubmed/20573942
- Lasisi AO, Fehintola FA, Yusuf OB. Age-related hearing loss, vitamin B12, and folate in the elderly. Otolaryngol Head Neck Surg. Dec 2010;143(6):826-30. doi:10.1016/j.otohns.2010.08.031. https://www.ncbi.nlm.nih.gov/pubmed/21109085
- Partearroyo T, Vallecillo N, Pajares MA, Varela-Moreiras G, Varela-Nieto I. Cochlear Homocysteine Metabolism at the Crossroad of Nutrition and Sensorineural Hearing Loss. Front Mol Neurosci. 2017;10:107. doi:10.3389/fnmol.2017.00107.
- Partearroyo T, Murillo-Cuesta S, Vallecillo N, et al. Betaine-homocysteine S-methyltransferase deficiency causes increased susceptibility to noise-induced hearing loss associated with plasma hyperhomocysteinemia. FASEB J. May 2019;33(5):5942-5956. doi:10.1096/fj.201801533R. https://www.ncbi.nlm.nih.gov/pubmed/30753104
- Szeto B, Valentini C, Lalwani AK. Low vitamin D status is associated with hearing loss in the elderly: a cross-sectional study. Am J Clin Nutr . Feb 2 2021;113(2):456-466. doi:10.1093/ajcn/nqaa310. https://www.ncbi.nlm.nih.gov/pubmed/33247302
- Bigman G. Deficiency in vitamin D is associated with bilateral hearing impairment and bilateral sensorineural hearing loss in older adults. Nutr Res . Sep 2022;105:1-10. doi:10.1016/j.nutres.2022.05.008. https://www.ncbi.nlm.nih.gov/pubmed/35779352
- Hosseini MS, Saeedi M, SA KH. Prevalence of Hearing Disorders among Type 2 Diabetes Mellitus Patients with and without Vitamin D Deficiency. Maedica (Bucur). Mar 2020;15(1):32-36. doi:10.26574/maedica.2020.15.1.32. https://www.ncbi.nlm.nih.gov/pubmed/32419858
- Bener A, Eliacik M, Cincik H, Ozturk M, DeFronzo RA, Abdul-Ghani M. The Impact of Vitamin D Deficiency on Retinopathy and Hearing Loss among Type 2 Diabetic Patients. Biomed Res Int. 2018;2018:2714590. doi:10.1155/2018/2714590. https://www.ncbi.nlm.nih.gov/pubmed/30112372
- Karaer I, Akalin Y. Low vitamin B12 level and vitamin D level adversely affect on cochlear health in women. Int J Vitam Nutr Res. Jun 2020;90(3-4):333-338. doi:10.1024/0300-9831/a000616. https://www.ncbi.nlm.nih.gov/pubmed/31623529
- Curhan SG, Eavey RD, Wang M, Rimm EB, Curhan GC. Fish and fatty acid consumption and the risk of hearing loss in women. Am J Clin Nutr. Nov 2014;100(5):1371-7. doi:10.3945/ajcn.114.091819. https://www.ncbi.nlm.nih.gov/pubmed/25332335
- Gopinath B, Flood VM, Rochtchina E, McMahon CM, Mitchell P. Consumption of omega-3 fatty acids and fish and risk of age-related hearing loss. Am J Clin Nutr. Aug 2010;92(2):416-21. doi:10.3945/ajcn.2010.29370. https://www.ncbi.nlm.nih.gov/pubmed/20534742
- Martinez-Vega R, Partearroyo T, Vallecillo N, Varela-Moreiras G, Pajares MA, Varela-Nieto I. Long-term omega-3 fatty acid supplementation prevents expression changes in cochlear homocysteine metabolism and ameliorates progressive hearing loss in C57BL/6J mice. J Nutr Biochem. Dec 2015;26(12):1424-33. doi:10.1016/j.jnutbio.2015.07.011. https://www.ncbi.nlm.nih.gov/pubmed/26321228
- Modanloo M, Shokrzadeh M. Analyzing Mitochondrial Dysfunction, Oxidative Stress, and Apoptosis: Potential Role of L-carnitine. Iran J Kidney Dis . Mar 2019;13(2):74-86.
- Alhasaniah AH. l-carnitine: Nutrition, pathology, and health benefits. Saudi J Biol Sci. Feb 2023;30(2):103555. doi:10.1016/j.sjbs.2022.103555. https://www.ncbi.nlm.nih.gov/pubmed/36632072
- Tokgoz SA, Vuralkan E, Sonbay ND, et al. Protective effects of vitamins E, B and C and L-carnitine in the prevention of cisplatin-induced ototoxicity in rats. J Laryngol Otol. May 2012;126(5):464-9. doi:10.1017/S0022215112000382. https://www.ncbi.nlm.nih.gov/pubmed/22490890
- Coleman JK, Kopke RD, Liu J, et al. Pharmacological rescue of noise induced hearing loss using N-acetylcysteine and acetyl-L-carnitine. Hear Res . Apr 2007;226(1-2):104-13. doi:10.1016/j.heares.2006.08.008. https://www.ncbi.nlm.nih.gov/pubmed/17023129
- Sha SH, Kanicki A, Halsey K, Wearne KA, Schacht J. Antioxidant-enriched diet does not delay the progression of age-related hearing loss. Neurobiol Aging . May 2012;33(5):1010 e15-6. doi:10.1016/j.neurobiolaging.2011.10.023. https://www.ncbi.nlm.nih.gov/pubmed/22154190
- Bielefeld EC, Coling D, Chen GD, Henderson D. Multiple dosing strategies with acetyl L-carnitine (ALCAR) fail to alter age-related hearing loss in the Fischer 344/NHsd rat. J Negat Results Biomed. Jul 11 2008;7:4. doi:10.1186/1477-5751-7-4. https://www.ncbi.nlm.nih.gov/pubmed/18620587
- Derin A, Agirdir B, Derin N, et al. The effects of L-carnitine on presbyacusis in the rat model. Clin Otolaryngol Allied Sci. Jun 2004;29(3):238-41. doi:10.1111/j.1365-2273.2004.00790.x. https://www.ncbi.nlm.nih.gov/pubmed/15142068
- Lasisi AO, Fehintola FA. Correlation between plasma levels of radical scavengers and hearing threshold among elderly subjects with age-related hearing loss. Acta Otolaryngol. Nov 2011;131(11):1160-4. doi:10.3109/00016489.2010.549840. https://www.ncbi.nlm.nih.gov/pubmed/21970786
- Liu J, Chen H, Lin X, et al. Melatonin Suppresses Cyclic GMP-AMP Synthase-Stimulator of Interferon Genes Signaling and Delays the Development of Hearing Loss in the C57BL/6J Presbycusis Mouse Model. Neuroscience . Jan 23 2023;doi:10.1016/j.neuroscience.2023.01.015. https://www.ncbi.nlm.nih.gov/pubmed/36702373
- Serra LSM, Araujo JG, Novanta G, et al. Melatonin prevents age-related hearing loss in the murin experimental model. Braz J Otorhinolaryngol . Nov-Dec 2022;88 Suppl 3(Suppl 3):S103-S108. doi:10.1016/j.bjorl.2022.06.002. https://www.ncbi.nlm.nih.gov/pubmed/35780011
- Bas E, Martinez-Soriano F, Lainez JM, Marco J. An experimental comparative study of dexamethasone, melatonin and tacrolimus in noise-induced hearing loss. Acta Otolaryngol. Apr 2009;129(4):385-9. doi:10.1080/00016480802566279. https://www.ncbi.nlm.nih.gov/pubmed/19051071
- Karlidag T, Yalcin S, Ozturk A, et al. The role of free oxygen radicals in noise induced hearing loss: effects of melatonin and methylprednisolone. Auris Nasus Larynx. Apr 2002;29(2):147-52. doi:10.1016/s0385-8146(01)00137-7. https://www.ncbi.nlm.nih.gov/pubmed/11893449
- Demir MG, Altintoprak N, Aydin S, Kosemihal E, Basak K. Effect of Transtympanic Injection of Melatonin on Cisplatin-Induced Ototoxicity. J Int Adv Otol. Dec 2015;11(3):202-6. doi:10.5152/iao.2015.1094. https://www.ncbi.nlm.nih.gov/pubmed/26915150
- Chen T, Luo Y, Li Q, et al. Melatonin reduces radiation damage in inner ear. Journal of radiation research. Mar 10 2021;62(2):217-225. doi:10.1093/jrr/rraa137. https://www.ncbi.nlm.nih.gov/pubmed/33454767
- Zhou X, Gao Y, Hu Y, Ma X. Melatonin protects cochlear hair cells from nicotine-induced injury through inhibiting apoptosis, inflammation, oxidative stress and endoplasmic reticulum stress. Basic Clin Pharmacol Toxicol . Oct 2021;129(4):308-318. doi:10.1111/bcpt.13638. https://www.ncbi.nlm.nih.gov/pubmed/34254721
- Phu HT, Thuan DTB, Nguyen THD, Posadino AM, Eid AH, Pintus G. Herbal Medicine for Slowing Aging and Aging-associated Conditions: Efficacy, Mechanisms and Safety. Curr Vasc Pharmacol. 2020;18(4):369-393. doi:10.2174/1570161117666190715121939. https://www.ncbi.nlm.nih.gov/pubmed/31418664
- Qi HY, Li L, Ma H. Cellular stress response mechanisms as therapeutic targets of ginsenosides. Medicinal research reviews. Mar 2018;38(2):625-654. doi:10.1002/med.21450. https://www.ncbi.nlm.nih.gov/pubmed/28586505
- Tian C, Kim YJ, Lim HJ, Kim YS, Park HY, Choung YH. Red ginseng delays age-related hearing and vestibular dysfunction in C57BL/6 mice. Exp Gerontol. Sep 2014;57:224-32. doi:10.1016/j.exger.2014.06.013. https://www.ncbi.nlm.nih.gov/pubmed/24952098
- Mungan Durankaya S, Olgun Y, Aktas S, et al. Effect of Korean Red Ginseng on Noise-Induced Hearing Loss. Turk Arch Otorhinolaryngol. Jun 2021;59(2):111-117. doi:10.4274/tao.2021.2021-1-5. https://www.ncbi.nlm.nih.gov/pubmed/34386797
- Chen XM, Ji SF, Liu YH, et al. Ginsenoside Rd Ameliorates Auditory Cortex Injury Associated With Military Aviation Noise-Induced Hearing Loss by Activating SIRT1/PGC-1alpha Signaling Pathway. Front Physiol. 2020;11:788. doi:10.3389/fphys.2020.00788. https://www.ncbi.nlm.nih.gov/pubmed/32792971
- Choung YH, Kim SW, Tian C, et al. Korean red ginseng prevents gentamicin-induced hearing loss in rats. Laryngoscope. Jun 2011;121(6):1294-302. doi:10.1002/lary.21756. https://www.ncbi.nlm.nih.gov/pubmed/21541943
- Tian CJ, Kim SW, Kim YJ, et al. Red ginseng protects against gentamicin-induced balance dysfunction and hearing loss in rats through antiapoptotic functions of ginsenoside Rb1. Food Chem Toxicol. Oct 2013;60:369-76. doi:10.1016/j.fct.2013.07.069. https://www.ncbi.nlm.nih.gov/pubmed/23933362
- Olgun Y, Kirkim G, Altun Z, et al. Protective Effect of Korean Red Ginseng on Cisplatin Ototoxicity: Is It Effective Enough? J Int Adv Otol. Aug 2016;12(2):177-183. doi:10.5152/iao.2016.1989. https://www.ncbi.nlm.nih.gov/pubmed/27487360
- Park SY, Seo JH, Kim JK, Park KH. Effects of korean red ginseng on hearing and blood glucose levels in steroid therapy for sudden sensorineural hearing loss. Clin Exp Otorhinolaryngol. Sep 2014;7(3):170-4. doi:10.3342/ceo.2014.7.3.170. https://www.ncbi.nlm.nih.gov/pubmed/25177431
- CDC. Centers for Disease Control and Prevention. How Do I Prevent Hearing Loss from Loud Noise? Updated 10/31/2022. Accessed 11/25/2022, https://www.cdc.gov/nceh/hearing_loss/how_do_i_prevent_hearing_loss.html
- Themann CL, Masterson EA. Occupational noise exposure: A review of its effects, epidemiology, and impact with recommendations for reducing its burden. J Acoust Soc Am. Nov 2019;146(5):3879. doi:10.1121/1.5134465. https://www.ncbi.nlm.nih.gov/pubmed/31795665
- NIDCD. National Institute on Deafness and Other Communication Disorders. Noise-Induced Hearing Loss. Updated 3/16/2022. Accessed 10/3/2022, https://www.nidcd.nih.gov/health/noise-induced-hearing-loss
- Kwak C, Han W. The Effectiveness of Hearing Protection Devices: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. Nov 7 2021;18(21)doi:10.3390/ijerph182111693. https://www.ncbi.nlm.nih.gov/pubmed/34770206
- CDC. Centers for Disease Control and Prevention. Study Finds Half of Noise-Exposed Workers Do Not Use Hearing Protection When Exposed to Noise on the Job. Updated 10/7/2021. Accessed 11/25/2022, https://www.cdc.gov/niosh/updates/upd-10-07-21.html
- CCOHS. Canadian Centre for Occupational Health and Safety. Hearing Protectors. Updated 1/8/2021. Accessed 11/25/2022, https://www.ccohs.ca/oshanswers/prevention/ppe/ear_prot.html
- Hoshina T, Fujiyama D, Koike T, Ikeda K. Effects of an Active Noise Control Technology Applied to Earphones on Preferred Listening Levels in Noisy Environments. J Audiol Otol. Jul 2022;26(3):122-129. doi:10.7874/jao.2021.00612. https://www.ncbi.nlm.nih.gov/pubmed/35316868
- Meng ZL, Chen F, Zhao F, Gu HL, Zheng Y. Early detection of noise-induced hearing loss. World J Clin Cases. Feb 26 2022;10(6):1815-1825. doi:10.12998/wjcc.v10.i6.1815. https://www.ncbi.nlm.nih.gov/pubmed/35317152
- Spankovich C, Le Prell CG. The role of diet in vulnerability to noise-induced cochlear injury and hearing loss. J Acoust Soc Am. Nov 2019;146(5):4033. doi:10.1121/1.5132707. https://www.ncbi.nlm.nih.gov/pubmed/31795697
- Frye MD, Ryan AF, Kurabi A. Inflammation associated with noise-induced hearing loss. J Acoust Soc Am. Nov 2019;146(5):4020. doi:10.1121/1.5132545. https://www.ncbi.nlm.nih.gov/pubmed/31795714
- Jung SY, Kim SH, Yeo SG. Association of Nutritional Factors with Hearing Loss. Nutrients. Feb 1 2019;11(2)doi:10.3390/nu11020307. https://www.ncbi.nlm.nih.gov/pubmed/30717210
- Yevenes-Briones H, Caballero FF, Struijk EA, Lana A, Rodriguez-Artalejo F, Lopez-Garcia E. Dietary fat intake and risk of disabling hearing impairment: a prospective population-based cohort study. Eur J Nutr . Feb 2022;61(1):231-242. doi:10.1007/s00394-021-02644-7. https://www.ncbi.nlm.nih.gov/pubmed/34287672
- Gopinath B, Flood VM, Teber E, McMahon CM, Mitchell P. Dietary intake of cholesterol is positively associated and use of cholesterol-lowering medication is negatively associated with prevalent age-related hearing loss. J Nutr. Jul 2011;141(7):1355-61. doi:10.3945/jn.111.138610. https://www.ncbi.nlm.nih.gov/pubmed/21613455
- Dawes P, Cruickshanks KJ, Marsden A, Moore DR, Munro KJ. Relationship Between Diet, Tinnitus, and Hearing Difficulties. Ear Hear. Mar/Apr 2020;41(2):289-299. doi:10.1097/AUD.0000000000000765. https://www.ncbi.nlm.nih.gov/pubmed/31356390
- Jung DJ, Lee JY, Cho KH, Lee KY, Do JY, Kang SH. Association between a High-Potassium Diet and Hearing Thresholds in the Korean Adult Population. Sci Rep. Jul 4 2019;9(1):9694. doi:10.1038/s41598-019-45930-5. https://www.ncbi.nlm.nih.gov/pubmed/31273228
- Li W, Peng Y, Chen D, Lu Z, Tao Y. Association of weight change across adulthood with hearing loss: A retrospective cohort study. Int J Obes (Lond) . Oct 2022;46(10):1825-1832. doi:10.1038/s41366-022-01197-x. https://www.ncbi.nlm.nih.gov/pubmed/35869275
- Rim HS, Kim MG, Park DC, et al. Association of Metabolic Syndrome with Sensorineural Hearing Loss. J Clin Med. Oct 22 2021;10(21)doi:10.3390/jcm10214866. https://www.ncbi.nlm.nih.gov/pubmed/34768385
- Hu H, Tomita K, Kuwahara K, et al. Obesity and risk of hearing loss: A prospective cohort study. Clin Nutr. Mar 2020;39(3):870-875. doi:10.1016/j.clnu.2019.03.020. https://www.ncbi.nlm.nih.gov/pubmed/30954364
- Ramatsoma H, Patrick SM. Hypertension Associated With Hearing Loss and Tinnitus Among Hypertensive Adults at a Tertiary Hospital in South Africa. Front Neurol. 2022;13:857600. doi:10.3389/fneur.2022.857600. https://www.ncbi.nlm.nih.gov/pubmed/35370902
- Martinez-Amezcua P, Dooley EE, Reed NS, et al. Association of Hearing Impairment and 24-Hour Total Movement Activity in a Representative Sample of US Adults. JAMA Netw Open. Mar 1 2022;5(3):e222983. doi:10.1001/jamanetworkopen.2022.2983. https://www.ncbi.nlm.nih.gov/pubmed/35302630
- Garcia Morales EE, Ting J, Gross AL, et al. Association of Cigarette Smoking Patterns Over 30 Years With Audiometric Hearing Impairment and Speech-in-Noise Perception: The Atherosclerosis Risk in Communities Study. JAMA Otolaryngol Head Neck Surg. Mar 1 2022;148(3):243-251. doi:10.1001/jamaoto.2021.3982. https://www.ncbi.nlm.nih.gov/pubmed/35084441
- Baiduc RR, Sun JW, Spankovich C, Vance EA. Tobacco, but Neither Cannabis Smoking Nor Co-Drug Use, Is Associated With Hearing Loss in the National Health and Nutrition Examination Survey, 2011 to 2012 and 2015 to 2016. Ear Hear. Sep-Oct 01 2022;43(5):1582-1592. doi:10.1097/AUD.0000000000001219. https://www.ncbi.nlm.nih.gov/pubmed/35383601
- Song JJ, Go YY, Mun JY, et al. Effect of electronic cigarettes on human middle ear. Int J Pediatr Otorhinolaryngol. Jun 2018;109:67-71. doi:10.1016/j.ijporl.2018.03.028. https://www.ncbi.nlm.nih.gov/pubmed/29728187
- Demir E, Topal S. Sudden sensorineural hearing loss associated with electronic cigarette liquid: The first case in the literature. Int J Pediatr Otorhinolaryngol . Nov 2018;114:26-28. doi:10.1016/j.ijporl.2018.08.019. https://www.ncbi.nlm.nih.gov/pubmed/30262362
- Smith RJ, Gooi A. Hearing loss in children: Etiology - UpToDate. UpToDate. Accessed 10/25/2022, https://www.uptodate.com/contents/hearing-loss-in-children-etiology
- Bowl MR, Dawson SJ. Age-Related Hearing Loss. Cold Spring Harbor perspectives in medicine . Aug 1 2019;9(8)doi:10.1101/cshperspect.a033217. https://www.ncbi.nlm.nih.gov/pubmed/30291149
- Bazard P, Pineros J, Frisina RD, et al. Cochlear Inflammaging in Relation to Ion Channels and Mitochondrial Functions. Cells. Oct 15 2021;10(10)doi:10.3390/cells10102761. https://www.ncbi.nlm.nih.gov/pubmed/34685743
- Kociszewska D, Vlajkovic S. Age-Related Hearing Loss: The Link between Inflammaging, Immunosenescence, and Gut Dysbiosis. Int J Mol Sci. Jul 1 2022;23(13)doi:10.3390/ijms23137348. https://www.ncbi.nlm.nih.gov/pubmed/35806352
- Kociszewska D, Vlajkovic SM. The Association of Inflammatory Gut Diseases with Neuroinflammatory and Auditory Disorders. Frontiers in bioscience (Elite edition). Mar 22 2022;14(2):8. doi:10.31083/j.fbe1402008. https://www.ncbi.nlm.nih.gov/pubmed/35730449
- Cui B, Su D, Li W, et al. Effects of chronic noise exposure on the microbiome-gut-brain axis in senescence-accelerated prone mice: implications for Alzheimer's disease. J Neuroinflammation. Jun 22 2018;15(1):190. doi:10.1186/s12974-018-1223-4. https://www.ncbi.nlm.nih.gov/pubmed/29933742
- Denton AJ, Godur DA, Mittal J, Bencie NB, Mittal R, Eshraghi AA. Recent Advancements in Understanding the Gut Microbiome and the Inner Ear Axis. Otolaryngol Clin North Am. Oct 2022;55(5):1125-1137. doi:10.1016/j.otc.2022.07.002. https://www.ncbi.nlm.nih.gov/pubmed/36088154
- Ding T, Yan A, Liu K. What is noise-induced hearing loss? Br J Hosp Med (Lond). Sep 2 2019;80(9):525-529. doi:10.12968/hmed.2019.80.9.525. https://www.ncbi.nlm.nih.gov/pubmed/31498679
- Seidman MD, Standring RT. Noise and quality of life. Int J Environ Res Public Health. Oct 2010;7(10):3730-8. doi:10.3390/ijerph7103730. https://www.ncbi.nlm.nih.gov/pubmed/21139857
- Hammer MS, Swinburn TK, Neitzel RL. Environmental noise pollution in the United States: developing an effective public health response. Environ Health Perspect. Feb 2014;122(2):115-9. doi:10.1289/ehp.1307272. https://www.ncbi.nlm.nih.gov/pubmed/24311120
- NIOSH. The National Institute for Occupational Safety and Health. Noise & Hearing Loss Prevention. Centers for Disease Control and Prevention. Updated 2/6/2018. Accessed 10/3/2022, https://www.cdc.gov/niosh/topics/noise/default.html
- CDC. Centers for Disease Control and Prevention. Public Health and Scientific Information. Loud Noise Can Cause Hearing Loss. Accessed 11/8/2022, https://www.cdc.gov/nceh/hearing_loss/public_health_scientific_info.html
- CDC. Centers for Disease Control and Prevention. Loud Noises Can Cause Hearing Loss. Updated 10/7/2019. Accessed 11/8/2022, https://www.cdc.gov/nceh/hearing_loss/what_noises_cause_hearing_loss.html
- Seidman MD, Khan MJ, Bai U, Shirwany N, Quirk WS. Biologic activity of mitochondrial metabolites on aging and age-related hearing loss. Am J Otol . Mar 2000;21(2):161-7. doi:10.1016/s0196-0709(00)80003-4. https://www.ncbi.nlm.nih.gov/pubmed/10733178
- Zaman M, Muslim M, Jehangir A. Environmental noise-induced cardiovascular, metabolic and mental health disorders: a brief review. Environ Sci Pollut Res Int . Nov 2022;29(51):76485-76500. doi:10.1007/s11356-022-22351-y. https://www.ncbi.nlm.nih.gov/pubmed/35931843
- Kurabi A, Keithley EM, Housley GD, Ryan AF, Wong AC. Cellular mechanisms of noise-induced hearing loss. Hear Res. Jun 2017;349:129-137. doi:10.1016/j.heares.2016.11.013. https://www.ncbi.nlm.nih.gov/pubmed/27916698
- Sevy JO, Hohman MH, Singh A. Cerumen Impaction Removal. StatPearls. StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022. https://www.ncbi.nlm.nih.gov/pubmed/28846265
- Ligezinski A. [Ototoxic complications of chemotherapy]. Polski merkuriusz lekarski : organ Polskiego Towarzystwa Lekarskiego. Feb 2002;12(68):147-51. Ototoksyczne powiklania chemioterapii. https://www.ncbi.nlm.nih.gov/pubmed/11995254
- Verdel BM, van Puijenbroek EP, Souverein PC, Leufkens HG, Egberts AC. Drug-related nephrotoxic and ototoxic reactions : a link through a predictive mechanistic commonality. Drug safety. 2008;31(10):877-84. doi:10.2165/00002018-200831100-00006. https://www.ncbi.nlm.nih.gov/pubmed/18759511
- Cone B, Dorn P, D K-M, Lister J, Ortiz C, Schairer K. Ototoxic Medications (Medication Effects). American Speech-Language-Hearing Association. Accessed 12/6/2022, https://www.asha.org/public/hearing/ototoxic-medications/
- Lustig LR. Herpes Zoster Oticus. Merck Manual Professional Version. Updated 9/2022. Accessed 12/6/2022, https://www.merckmanuals.com/professional/ear,-nose,-and-throat-disorders/inner-ear-disorders/herpes-zoster-oticus
- Warren B, Fenton GE, Klenschi E, Windmill JFC, French AS. Physiological Basis of Noise-Induced Hearing Loss in a Tympanal Ear. J Neurosci. Apr 8 2020;40(15):3130-3140. doi:10.1523/JNEUROSCI.2279-19.2019. https://www.ncbi.nlm.nih.gov/pubmed/32144181
- Salmon MK, Brant J, Hohman MH, Leibowitz D. Audiogram Interpretation. StatPearls . 2022. https://www.ncbi.nlm.nih.gov/pubmed/35201707
- Menzel OJ. Audiogram interpretation. III. Eye Ear Nose Throat Mon . Mar 1963;42:78-81 contd. https://www.ncbi.nlm.nih.gov/pubmed/13934898
- Klyn NAM, Letendre C, Shrestha N, Lambert BL, Dhar S. Interpretability of the audiogram by audiologists and physician non-specialists. Int J Audiol. Feb 2021;60(2):133-139. doi:10.1080/14992027.2020.1805129. https://www.ncbi.nlm.nih.gov/pubmed/32815399
- American Speech-Language-Hearing Association. Learning About Hearing Aids. Updated 2015. https://www.asha.org/siteassets/ais/ais-learning-hearing-aids.pdf
- NIH. National Institute on Deafness and Other Communication Disorders. Hearing Aids. Updated 10/11/2022. Accessed 11/8/2022, https://www.nidcd.nih.gov/health/hearing-aids#hearingaid_06
- FDA. U.S. Food and Drug Administration. Hearing Aids and Personal Sound Amplification Products: What to Know. Available at https://www.fda.gov/consumers/consumer-updates/hearing-aids-and-personal-sound-amplification-products-what-know Updated 01/12/2023. Accessed 03/02/2023. Accessed 11/11/2022,
- University OHS. Ears, Nose & Throat. Types of Hearing Aids. Accessed 11/11/2022, https://www.ohsu.edu/ent/types-hearing-aids
- FDA. FDA Finalizes Historic Rule Enabling Access to Over-the-Counter Hearing Aids for Millions of Americans | FDA. @US_FDA. Updated Tue, 08/16/2022 - 09:00. https://www.fda.gov/news-events/press-announcements/fda-finalizes-historic-rule-enabling-access-over-counter-hearing-aids-millions-americans
- Schmidt C. National Council on Aging. The 12 Best Hearing Aids of 2022. Updated 11/7/2022. Accessed 11/11/2022, https://www.ncoa.org/adviser/hearing-aids/best-hearing-aids/
- Simpson BW. The Hearing Aid Revolution: Cheaper and Easier to Get. Johns Hopkins Bloomberg School of Public Health. Updated 10/22/2021. Accessed 11/11/2022, https://publichealth.jhu.edu/2021/the-hearing-aid-revolution-cheaper-and-easier-to-get
- Everett C. National Council on Aging. The 6 Most Affordable Hearing Aids of 2022. Updated 11/7/2022. Accessed 11/11/2022, https://www.ncoa.org/adviser/hearing-aids/best-affordable-hearing-aids/
- NIH. National Institutes of Health: Naitonal Institute on Deafness and Other Communication Disorders. Assistive Devices for People with Hearing, Voice, Speech, or Language Disorders. Available at https://www.nidcd.nih.gov/health/assistive-devices-people-hearing-voice-speech-or-language-disorders Last updated 11/12/2019. Accessed 03/03/2023. 2019;
- Hearing Loss Association of America. Assistive Listening Systems. 11/11/2022. https://www.hearingloss.org/hearing-help/technology/hat/alds/
- National Association of the Deaf. Assistive Listening Systems and Devices. Accessed 11/11/2022, https://www.nad.org/resources/technology/assistive-listening/assistive-listening-systems-and-devices/
- Department of Human Services. Deaf and Hard of Hearing Services Division. Assistive listening devices. Accessed 11/11/2022, https://mn.gov/deaf-hard-of-hearing/assistive-technology/assistive-listening-devices/
- Roche JP, Hansen MR. On the Horizon: Cochlear Implant Technology. Otolaryngol Clin North Am . Dec 2015;48(6):1097-116. doi:10.1016/j.otc.2015.07.009. https://www.ncbi.nlm.nih.gov/pubmed/26443490
- Babajanian EE, Patel NS, Gurgel RK. The Impact of Cochlear Implantation: Cognitive Function, Quality of Life, and Frailty in Older Adults. Semin Hear. Nov 2021;42(4):342-351. doi:10.1055/s-0041-1739367. https://www.ncbi.nlm.nih.gov/pubmed/34912162
- Lally JW, Adams JK, Wilkerson BJ. The use of cochlear implantation in the elderly. Curr Opin Otolaryngol Head Neck Surg. Oct 2019;27(5):387-391. doi:10.1097/MOO.0000000000000569. https://www.ncbi.nlm.nih.gov/pubmed/31460986
- FDA. Food and Drug Adminstration. Cochlear Implants. Accessed 10/3/2022, https://www.fda.gov/medical-devices/implants-and-prosthetics/cochlear-implants
- FDA. US Food & Drug Administration. Types of Hearing Aids. Available at https://www.fda.gov/medical-devices/hearing-aids/types-hearing-aids Updated 11/14/2022. Accessed 03/02/2023. 2022;
- ASU Speech and Hearing Clinic. Advantages and Disadvantages of Assistive Listening Devices. Ariozna Statue University College of Health Solutions. Accessed May 2, 2023, https://asuspeechandhearingclinic.org/hearing/rehabilitation-services/assistive-listening-devices/what-are-assistive-listening-devices/advantages-and-disadvantages-assistive-listening-devices
- Radford JC. Treatment of impacted ear wax: a case for increased community-based microsuction. BJGP Open. Jun 2020;4(2)doi:10.3399/bjgpopen20X101064. https://www.ncbi.nlm.nih.gov/pubmed/32238391
- Michaudet C, Malaty J. Cerumen Impaction: Diagnosis and Management. Am Fam Physician. Oct 15 2018;98(8):525-529. https://www.ncbi.nlm.nih.gov/pubmed/30277727
- Schumann JA, Toscano ML, Pfleghaar N. Ear Irrigation. StatPearls. StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022. https://www.ncbi.nlm.nih.gov/pubmed/29083577
- Cedars-Sinai. Is It Really Dangerous to Clean My Ears with Cotton Swabs? Updated 8/1/2018. Accessed 10/3/2022, https://www.cedars-sinai.org/blog/is-it-really-dangerous-to-clean-my-ears-with-cotton-swabs.html
- Cleveland Clinic. Earwax Removal 101: The Best (and Safest) Ways to Clear Clogged Ears. Updated 11/29/2021. Accessed 11/8/2022, https://health.clevelandclinic.org/ear-wax-removal-101-the-best-and-safest-ways-to-clear-clogged-ears/
- Limb CJ, Lustig LR, Durand ML. Acute otitis media in adults. UpToDate. Updated 4/6/2022. Accessed 11/8/2022, https://www.uptodate.com/contents/acute-otitis-media-in-adults
- Pelton SI, Tähtinen P. Acute otitis media in children: Treatment. UpToDate. Updated 10/3/2022. Accessed 11/8/2022, https://www.uptodate.com/contents/acute-otitis-media-in-children-treatment
- Barkwill D, Arora R. Labyrinthitis. StatPearls. StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022. https://www.ncbi.nlm.nih.gov/pubmed/32809341
- Rudic M, Keogh I, Wagner R, et al. The pathophysiology of otosclerosis: Review of current research. Hear Res. Dec 2015;330(Pt A):51-6. doi:10.1016/j.heares.2015.07.014. https://www.ncbi.nlm.nih.gov/pubmed/26276418
- Mangia LRL, Coelho LOM, Carvalho B, de Oliveira AKP, Hamerschmidt R. Imaging Studies in Otosclerosis: An Up-to-date Comprehensive Review. Int Arch Otorhinolaryngol. Apr 2021;25(2):e318-e327. doi:10.1055/s-0040-1715149. https://www.ncbi.nlm.nih.gov/pubmed/33968239
- de Oliveira Penido N, de Oliveira Vicente A. Medical Management of Otosclerosis. Otolaryngol Clin North Am. Apr 2018;51(2):441-452. doi:10.1016/j.otc.2017.11.006. https://www.ncbi.nlm.nih.gov/pubmed/29502728
- Yu H, He Y, Ni Y, Wang Y, Lu N, Li H. PORP vs. TORP: a meta-analysis. Eur Arch Otorhinolaryngol. Nov 2013;270(12):3005-17. doi:10.1007/s00405-013-2388-1. https://www.ncbi.nlm.nih.gov/pubmed/23400405
- Wegner I, van den Berg JW, Smit AL, Grolman W. Systematic review of the use of bone cement in ossicular chain reconstruction and revision stapes surgery. Laryngoscope. Jan 2015;125(1):227-33. doi:10.1002/lary.24897. https://www.ncbi.nlm.nih.gov/pubmed/25154873
- Koleilat A, Driscoll CLW, Schimmenti LA, Poling GL. Emerging Therapies and Approaches to Treat and Prevent Hearing Loss. Perspectives of the ASHA Special Interest Groups. 2020;5(5):1147-1165. doi:10.1044/2020_persp-20-00072. https://pubs.asha.org/doi/abs/10.1044/2020_PERSP-20-00072
- Glantz G. Gene Therapy for Hearing Loss on the Horizon. The Hearing Journal. 2022;75(1):14,15,16. doi:10.1097/01.Hj.0000812688.91831.57. https://journals.lww.com/thehearingjournal/Fulltext/2022/01000/Gene_Therapy_for_Hearing_Loss_on_the_Horizon.1.aspx
- Chai R, Li H, Yang T, Sun S, Yuan Y. Editorial: Hearing Loss: Mechanisms and Prevention. Editorial. Frontiers in cell and developmental biology. 2022-February-03 2022;10:838271. doi:10.3389/fcell.2022.838271. https://www.ncbi.nlm.nih.gov/pubmed/35186939
- He Z, Kong W, Zou S, Huang H, Sha S. Editorial: Hearing Loss: From Pathogenesis to Treatment. Front Cell Neurosci. 2022;16:907483. doi:10.3389/fncel.2022.907483. https://www.ncbi.nlm.nih.gov/pubmed/35755783
- Ortega MA, Fraile-Martinez O, Garcia-Montero C, et al. A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities. Medicina (Kaunas). Aug 24 2021;57(9)doi:10.3390/medicina57090864. https://www.ncbi.nlm.nih.gov/pubmed/34577787
- Joshua TG, Ayub A, Wijesinghe P, Nunez DA. Hyperbaric Oxygen Therapy for Patients With Sudden Sensorineural Hearing Loss: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. Jan 1 2022;148(1):5-11. doi:10.1001/jamaoto.2021.2685. https://www.ncbi.nlm.nih.gov/pubmed/34709348
- John Hopkins Medicine. Hyperbaric Oxygen Therapy. Accessed 2/21/2023, https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/hyperbaric-oxygen-therapy#:~:text=For%20this%20therapy%2C%20you%20enter%20a%20special%20chamber%20to%20breathe%20in%20pure%20oxygen%20in%20air%20pressure%20levels%201.5%20to%C2%A03%20times%20higher%20than%20average
- Cavaliere M, De Luca P, Scarpa A, et al. Combination of Hyperbaric Oxygen Therapy and Oral Steroids for the Treatment of Sudden Sensorineural Hearing Loss: Early or Late? Medicina (Kaunas). Oct 10 2022;58(10)doi:10.3390/medicina58101421. https://www.ncbi.nlm.nih.gov/pubmed/36295581
- Whitlon DS. Statins and hearing. Hear Res. Nov 2022;425:108453. doi:10.1016/j.heares.2022.108453. https://www.ncbi.nlm.nih.gov/pubmed/35125240
- Yucel H, Yucel A, Arbag H, Cure E, Eryilmaz MA, Ozer AB. Effect of statins on hearing function and subjective tinnitus in hyperlipidemic patients. Romanian journal of internal medicine = Revue roumaine de medecine interne. Jun 1 2019;57(2):133-140. doi:10.2478/rjim-2018-0035. https://www.ncbi.nlm.nih.gov/pubmed/30447148
- Olzowy B, Canis M, Hempel JM, Mazurek B, Suckfull M. Effect of atorvastatin on progression of sensorineural hearing loss and tinnitus in the elderly: results of a prospective, randomized, double-blind clinical trial. Otol Neurotol. Jun 2007;28(4):455-8. doi:10.1097/01.mao.0000271673.33683.7b. https://www.ncbi.nlm.nih.gov/pubmed/17529847
- Kim SY, Lee CH, Min C, Yoo DM, Choi HG. Association between statin medication and hearing impairment in a national health screening cohort. Sci Rep. Jul 13 2021;11(1):14388. doi:10.1038/s41598-021-93916-z. https://www.ncbi.nlm.nih.gov/pubmed/34257355
- Chung SD, Chen CH, Hung SH, Lin HC, Wang LH. A population-based study on the association between statin use and sudden sensorineural hearing loss. Otolaryngol Head Neck Surg. Feb 2015;152(2):319-25. doi:10.1177/0194599814559382. https://www.ncbi.nlm.nih.gov/pubmed/25450412
- Han HW, Yee J, Park YH, Gwak HS. Association between Statin Use and Sensorineural Hearing Loss in Type 2 Diabetic Patients: A Hospital-Based Study. Pharmaceuticals (Basel). Oct 25 2021;14(11)doi:10.3390/ph14111076. https://www.ncbi.nlm.nih.gov/pubmed/34832858
- Fernandez KA, Allen P, Campbell M, et al. Atorvastatin is associated with reduced cisplatin-induced hearing loss. J Clin Invest. Jan 4 2021;131(1)doi:10.1172/JCI142616. https://www.ncbi.nlm.nih.gov/pubmed/33393488
- Kil J, Harruff EE, Longenecker RJ. Development of ebselen for the treatment of sensorineural hearing loss and tinnitus. Hear Res. Jan 2022;413:108209. doi:10.1016/j.heares.2021.108209. https://www.ncbi.nlm.nih.gov/pubmed/33678494
- Kil J, Lobarinas E, Spankovich C, et al. Safety and efficacy of ebselen for the prevention of noise-induced hearing loss: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. Sep 2 2017;390(10098):969-979. doi:10.1016/S0140-6736(17)31791-9. https://www.ncbi.nlm.nih.gov/pubmed/28716314
- ClinicalTrials.gov. SPI-1005 for the Treatment of Meniere's Disease (STOPMD-3). Updated 7/29/2022. Accessed 10/3/2022, https://clinicaltrials.gov/ct2/show/NCT04677972
- Nourbakhsh A, Colbert BM, Nisenbaum E, et al. Stem Cells and Gene Therapy in Progressive Hearing Loss: the State of the Art. J Assoc Res Otolaryngol. Apr 2021;22(2):95-105. doi:10.1007/s10162-020-00781-0. https://www.ncbi.nlm.nih.gov/pubmed/33507440
- He Z, Ding Y, Mu Y, et al. Stem Cell-Based Therapies in Hearing Loss. Frontiers in cell and developmental biology. 2021;9:730042. doi:10.3389/fcell.2021.730042. https://www.ncbi.nlm.nih.gov/pubmed/34746126
- Matsuoka AJ, Morrissey ZD, Zhang C, et al. Directed Differentiation of Human Embryonic Stem Cells Toward Placode-Derived Spiral Ganglion-Like Sensory Neurons. Stem cells translational medicine. Mar 2017;6(3):923-936. doi:10.1002/sctm.16-0032. https://www.ncbi.nlm.nih.gov/pubmed/28186679
- Sakano H, Harris JP. Emerging options in immune-mediated hearing loss. Laryngoscope Investig Otolaryngol. Feb 2019;4(1):102-108. doi:10.1002/lio2.205. https://www.ncbi.nlm.nih.gov/pubmed/30828626
- Seidman MD, Tang W, Shirwany N, et al. Anti-intercellular adhesion molecule-1 antibody's effect on noise damage. Laryngoscope. Apr 2009;119(4):707-12. doi:10.1002/lary.20109. https://www.ncbi.nlm.nih.gov/pubmed/19213042
- Seidman MD, Van De Water TR. Pharmacologic manipulation of the labyrinth with novel and traditional agents delivered to the inner ear. Ear Nose Throat J. Apr 2003;82(4):276-80, 282-3, 287-8 passim. https://www.ncbi.nlm.nih.gov/pubmed/12735160
- Foster AC, Jacques BE, Piu F. Hearing loss: The final frontier of pharmacology. Pharmacol Res Perspect. Jun 2022;10(3):e00970. doi:10.1002/prp2.970. https://www.ncbi.nlm.nih.gov/pubmed/35599339
- Slade K, Reilly JH, Jablonska K, et al. The impact of age-related hearing loss on structural neuroanatomy: A meta-analysis. Front Neurol. 2022;13:950997. doi:10.3389/fneur.2022.950997. https://www.ncbi.nlm.nih.gov/pubmed/36003293
- Ford AH, Hankey GJ, Yeap BB, Golledge J, Flicker L, Almeida OP. Hearing loss and the risk of dementia in later life. Maturitas. Jun 2018;112:1-11. doi:10.1016/j.maturitas.2018.03.004. https://www.ncbi.nlm.nih.gov/pubmed/29704910
- Babajanian EE, Gurgel RK. Cognitive and behavioral effects of hearing loss. Curr Opin Otolaryngol Head Neck Surg. Oct 1 2022;30(5):339-343. doi:10.1097/MOO.0000000000000825. https://www.ncbi.nlm.nih.gov/pubmed/36004783
- Nadhimi Y, Llano DA. Does hearing loss lead to dementia? A review of the literature. Hear Res. Mar 15 2021;402:108038. doi:10.1016/j.heares.2020.108038. https://www.ncbi.nlm.nih.gov/pubmed/32814645
- Slade K, Plack CJ, Nuttall HE. The Effects of Age-Related Hearing Loss on the Brain and Cognitive Function. Trends Neurosci. Oct 2020;43(10):810-821. doi:10.1016/j.tins.2020.07.005. https://www.ncbi.nlm.nih.gov/pubmed/32826080
- Loughrey DG, Kelly ME, Kelley GA, Brennan S, Lawlor BA. Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg . Feb 1 2018;144(2):115-126. doi:10.1001/jamaoto.2017.2513. https://www.ncbi.nlm.nih.gov/pubmed/29222544
- Powell DS, Oh ES, Reed NS, Lin FR, Deal JA. Hearing Loss and Cognition: What We Know and Where We Need to Go. Review. Front Aging Neurosci. 2022-February-28 2021;13:769405. doi:10.3389/fnagi.2021.769405. https://www.ncbi.nlm.nih.gov/pubmed/35295208
- Lee HJ, Joo YH, Han KD, Park KH. Association between Hearing Loss and Cognitive Disorder: A Nationwide Population-Based Study. Yonsei medical journal. May 2021;62(5):446-452. doi:10.3349/ymj.2021.62.5.446. https://www.ncbi.nlm.nih.gov/pubmed/33908216
- Bisogno A, Scarpa A, Di Girolamo S, et al. Hearing Loss and Cognitive Impairment: Epidemiology, Common Pathophysiological Findings, and Treatment Considerations. Life (Basel). Oct 17 2021;11(10):1102. doi:10.3390/life11101102. https://www.ncbi.nlm.nih.gov/pubmed/34685474
- Cosh S, Helmer C, Delcourt C, Robins TG, Tully PJ. Depression in elderly patients with hearing loss: current perspectives. Clin Interv Aging . 2019;14:1471-1480. doi:10.2147/CIA.S195824. https://www.ncbi.nlm.nih.gov/pubmed/31616138
- Lawrence BJ, Jayakody DMP, Bennett RJ, Eikelboom RH, Gasson N, Friedland PL. Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-analysis. The Gerontologist. Apr 2 2020;60(3):e137-e154. doi:10.1093/geront/gnz009. https://www.ncbi.nlm.nih.gov/pubmed/30835787
- Powell DS, Brenowitz WD, Yaffe K, et al. Examining the Combined Estimated Effects of Hearing Loss and Depressive Symptoms on Risk of Cognitive Decline and Incident Dementia. The journals of gerontology Series B, Psychological sciences and social sciences. May 5 2022;77(5):839-849. doi:10.1093/geronb/gbab194. https://www.ncbi.nlm.nih.gov/pubmed/34655295
- Kim AS, Garcia Morales EE, Amjad H, et al. Association of Hearing Loss With Neuropsychiatric Symptoms in Older Adults With Cognitive Impairment. Am J Geriatr Psychiatry. Jun 2021;29(6):544-553. doi:10.1016/j.jagp.2020.10.002. https://www.ncbi.nlm.nih.gov/pubmed/33168388
- Kiely KM, Anstey KJ, Luszcz MA. Dual sensory loss and depressive symptoms: the importance of hearing, daily functioning, and activity engagement. Front Hum Neurosci. 2013;7:837. doi:10.3389/fnhum.2013.00837. https://www.ncbi.nlm.nih.gov/pubmed/24379769
- Kuang D, Yu YY, Tu C. Bilateral high-frequency hearing loss is associated with elevated blood pressure and increased hypertension risk in occupational noise exposed workers. PLoS One. 2019;14(9):e0222135. doi:10.1371/journal.pone.0222135. https://www.ncbi.nlm.nih.gov/pubmed/31487326
- Cheng YF, Xirasagar S, Yang TH, Kuo NW, Lin HC. Association of hearing loss with land transport accidents: a nationwide population-based study. Int J Audiol. Sep 2022;61(9):731-735. doi:10.1080/14992027.2021.1998677. https://www.ncbi.nlm.nih.gov/pubmed/34772305
- Sakurai R, Suzuki H, Ogawa S, Takahashi M, Fujiwara Y. Hearing loss and increased gait variability among older adults. Gait Posture. Jun 2021;87:54-58. doi:10.1016/j.gaitpost.2021.04.007. https://www.ncbi.nlm.nih.gov/pubmed/33892392
- Consequences of Untreated Hearing Loss. https://betterhearing.org/your-hearing-health/consequences-of-untreated-hearing-loss/
- Lieu JEC, Kenna M, Anne S, Davidson L. Hearing Loss in Children: A Review. JAMA. Dec 1 2020;324(21):2195-2205. doi:10.1001/jama.2020.17647. https://www.ncbi.nlm.nih.gov/pubmed/33258894
- Pisoni DB, Kronenberger WG, Roman AS, Geers AE. Measures of digit span and verbal rehearsal speed in deaf children after more than 10 years of cochlear implantation. Ear Hear. Feb 2011;32(1 Suppl):60S-74S. doi:10.1097/AUD.0b013e3181ffd58e. https://www.ncbi.nlm.nih.gov/pubmed/21832890
- Teasdale TW, Sorensen MH. Hearing loss in relation to educational attainment and cognitive abilities: a population study. Int J Audiol. Apr 2007;46(4):172-5. doi:10.1080/14992020601089484. https://www.ncbi.nlm.nih.gov/pubmed/17454229
- Bigler D, Burke K, Laureano N, Alfonso K, Jacobs J, Bush ML. Assessment and Treatment of Behavioral Disorders in Children with Hearing Loss: A Systematic Review. Otolaryngol Head Neck Surg. Jan 2019;160(1):36-48. doi:10.1177/0194599818797598. https://www.ncbi.nlm.nih.gov/pubmed/30200810
- Dehankar SS, Gaurkar SS. Impact on Hearing Due to Prolonged Use of Audio Devices: A Literature Review. Cureus. Nov 2022;14(11):e31425. doi:10.7759/cureus.31425. https://www.ncbi.nlm.nih.gov/pubmed/36523704
- Bucholc M, Bauermeister S, Kaur D, McClean PL, Todd S. The impact of hearing impairment and hearing aid use on progression to mild cognitive impairment in cognitively healthy adults: An observational cohort study. Alzheimers Dement (N Y). 2022;8(1):e12248. doi:10.1002/trc2.12248. https://www.ncbi.nlm.nih.gov/pubmed/35229022
- SSA. Social Security Administration. Disability Evaluation Under Social Security: 2.00 Special Senses and Speech - Adult. Available at https://www.ssa.gov/disability/professionals/bluebook/2.00-SpecialSensesandSpeech-Adult.htm#2_10 Accessed 03/03/2023. 2023;
- WHO. World Health Organization. Deafness and Hearing Loss. Available at https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss Updated 02/27/2023. Accessed 03/03/2023. 2023;
- Hong SA, Kuziez D, Das N, Harris D, Brunworth JD. Hazardous sound outputs of white noise devices intended for infants. Int J Pediatr Otorhinolaryngol. Jul 2021;146:110757. doi:10.1016/j.ijporl.2021.110757. https://www.ncbi.nlm.nih.gov/pubmed/33992973
- MC. Mayo Clinic. Hearing Loss. Available at https://www.mayoclinic.org/diseases-conditions/hearing-loss/symptoms-causes/syc-20373072 Updated 04/16/2021. Accessed 03/03/2023. 2021;
- Tripathi P, Deshmukh P. Sudden Sensorineural Hearing Loss: A Review. Cureus . Sep 2022;14(9):e29458. doi:10.7759/cureus.29458. https://www.ncbi.nlm.nih.gov/pubmed/36299969
- Han BI, Lee HW, Ryu S, Kim JS. Tinnitus Update. J Clin Neurol. Jan 2021;17(1):1-10. doi:10.3988/jcn.2021.17.1.1. https://www.ncbi.nlm.nih.gov/pubmed/33480192
- Shearer AE, Hildebrand MS, Smith RJH. Hereditary Hearing Loss and Deafness Overview. In: Adam MP, Everman DB, Mirzaa GM, et al, eds. GeneReviews((R)). University of Washington, Seattle Copyright © 1993-2023, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved.; 1993. https://www.ncbi.nlm.nih.gov/pubmed/20301607
- Wells HRR, Newman TA, Williams FMK. Genetics of age-related hearing loss. Journal of neuroscience research. Sep 2020;98(9):1698-1704. doi:10.1002/jnr.24549. https://www.ncbi.nlm.nih.gov/pubmed/31989664